We present the case of a patient who underwent percutaneous coronary intervention (PCI) for left main trunk (LMT) bifurcation with a severely calcified lesion.
A 70-year-old man presented with effort angina. A calcified lesion was observed in the LMT bifurcation on optical coherence tomography (OCT) after dilation using a 2 mm semicompliant balloon (Figure 1A, Moving image 1, Moving image 2). The intima of the contralateral side of the calcified lesion was normal. After determining the ablation range using OCT, orbital atherectomy (OA) was performed using a Diamondback 360 Coronary Orbital Atherectomy System (OAS) (Cardiovascular Systems). Orbital atherectomy was performed three times at a low revolution speed (80,000 rpm). Subsequent angiography revealed that the wire bias approached the calcification. Furthermore, OCT revealed that the OAS penetrated the calcified nodule (Figure 1B). The OAS was then advanced through the lesion five times at a high speed (120,000 rpm). Subsequent OCT revealed that the wire had penetrated the calcification and that an oval-shaped portion had been removed (Figure 1C, Moving image 3). However, a substantial amount of calcification remained, and further debulking would likely have been difficult using the OAS. Therefore, rotational atherectomy (RA) was performed using a 2.0 mm ROTAPRO RA System (Boston Scientific) at 180,000 rpm. OCT revealed a deeper, circular groove in the calcified nodule (Figure 1D, Moving image 4, Moving image 5). After additional high-pressure cutting balloon dilatation (2.75/10 mm WOLVERINE; Boston Scientific), OCT confirmed sufficient luminal gain without major dissections. Coronary stent implantation was determined unnecessary, and a drug-coated balloon (DCB) (3.0/15 mm SeQuent Please NEO; B.Braun) was used to complete the procedure (Moving image 6, Moving image 7, Supplementary Figure 1).
To the best of our knowledge, the efficacy of combining OA and RA in bifurcation lesions has not been reported. In addition, only a few studies have reported the combined use of OA and RA for heavily calcified lesions in general1. PCI for highly calcified lesions has several issues, including negative long-term results, complexity of the procedure, complications, and a relatively low success rate. OA can be used in addition to conventional RA for highly calcified lesions, and the frequency of its use has been reportedly increasing2. The efficacy of OA in highly calcified lesions at bifurcation points has also been reported recently34.
In this case, the contralateral side of the calcified lesion was normal, and caution was required to avoid vascular injury due to atherectomy. Using unidirectional OA ablation, bias was applied only toward the lesion, and the procedure could be performed safely. By introducing a rotary burr into the lumen created by OA, RA was effective in obtaining further luminal gain. This case finding suggests that combining OA and RA, with appropriate lesion evaluation using imaging, could permit the safe and effective removal of severely calcified bifurcation nodules.
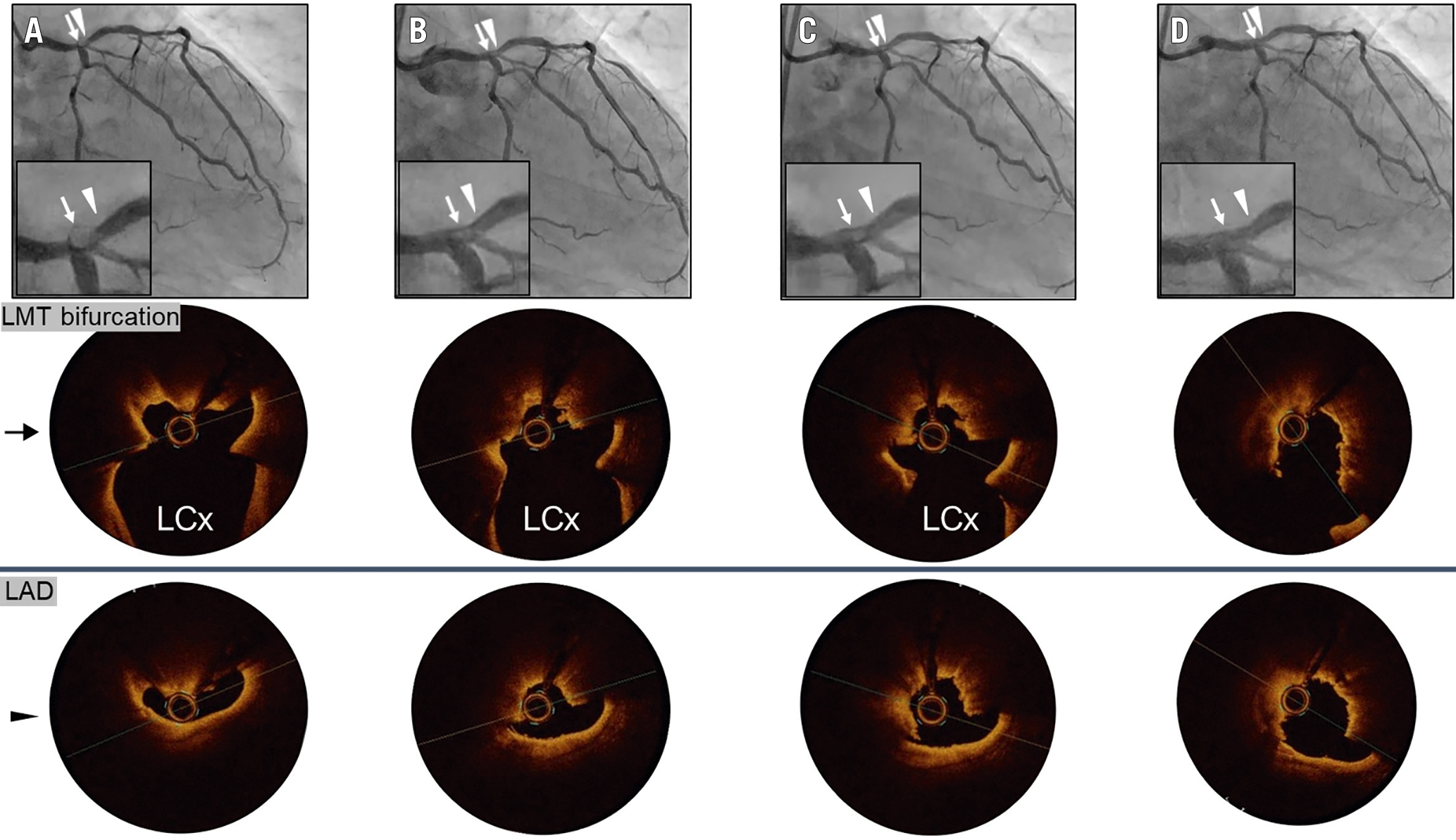
Figure 1. CAG and OCT findings. OCT images showing the left main trunk bifurcation (arrows) and left anterior descending ostium (arrowheads). A) CAG and OCT showing a calcified nodule in the bifurcation lesion. B) OCT showing a new groove in the calcified nodule following OA at low revolution speed. C) OCT showing that the groove penetrated deeper toward the centre of the nodule following OA at high-speed revolution. D) OCT indicating a larger lumen area following RA with a 2.00 mm burr. CAG: coronary angiography; LAD: left anterior descending artery; LCx: left circumflex artery; LMT: left main trunk; OA: orbital atherectomy; OCT: optical coherence tomography; RA: rotational atherectomy
Conflict of interest statement
The authors have no conficts of interest to declare.

