A 74-year-old male chronic smoker presented with chest discomfort of 10 hours duration. The first-contact 12-lead electrocardiogram (ECG) showed anterior wall ST-segment elevation myocardial infarction (STEMI). The patient was transported to the catheterisation laboratory for primary percutaneous coronary intervention (PCI), where an emergency angiography was performed through the right femoral artery approach. The left coronary angiogram showed the proper left anterior descending artery (LAD) arising from the left main coronary artery (Moving image 1). This LAD was short and terminated prematurely in the proximal anterior interventricular sulcus (AIVS) after diverting into a second diagonal branch which continued further down towards the apex. The left circumflex coronary artery was normally sized, arising from the left main coronary artery, and had a non-critical lesion. An angiography of the right coronary artery (RCA) showed a dominant RCA with non-significant stenosis and another vessel arising from its proximal segment (Moving image 2). This vessel travelled through to the left side to reach the anterior interventricular septum and had a septal branch as well as a third diagonal branch which was totally occluded in its ostio-proximal portion. The second LAD continued to the apex of the heart. This was consistent with the type IV variety of dual LAD. Another computed tomography (CT) evaluation of the anomalous LAD was carried out during the patient’s hospital stay; in this evaluation, the second LAD was seen arising from the proximal RCA, following an interarterial course, and reaching the epicardial position at the mid-septum. It supplied the mid- and distal portion of the septum and had a large septal branch and a third diagonal branch. The proximal portion of the third diagonal branch showed non-calcified plaque causing total occlusion (Figure 1).
The patient was managed conservatively, because the vessel was deemed to be of small calibre at the time of primary PCI, hence the patient received medical therapy. He remained asymptomatic and haemodynamically stable during the hospital stay. Given the anomalous anatomy of the coronary artery, coronary CT was performed which showed the LAD following a malignant course. The case was discussed with the cardiac surgery team and a coronary artery bypass graft (CABG) was recommended, but the patient refused any further intervention and was, therefore, put on optimal guideline-directed medical therapy.
The prevalence of dual LAD has been described as 1%, of which the rarest form of type IV dual LAD, in which the long LAD originates from the RCA, occurs in an estimated 0.004% of patients undergoing coronary angiography12. The risk correlated with a coronary artery anomaly usually depends on its location and course. The interarterial course is associated with more severe prognosis and increased risk of sudden cardiac death3.
Anomalous coronaries are rare and important, since they can potentially lead to confusion on the angiogram. This rare anomaly can lead to confusion where a “short LAD” artery may be misdiagnosed as a total occlusion and the long LAD as a conus branch. Awareness and recognition of anomalous coronaries are important for clinicians when planning revascularisation. Further advanced anatomical evaluation of coronary artery anomalies is often required for risk stratification and aiding in treatment decisions.
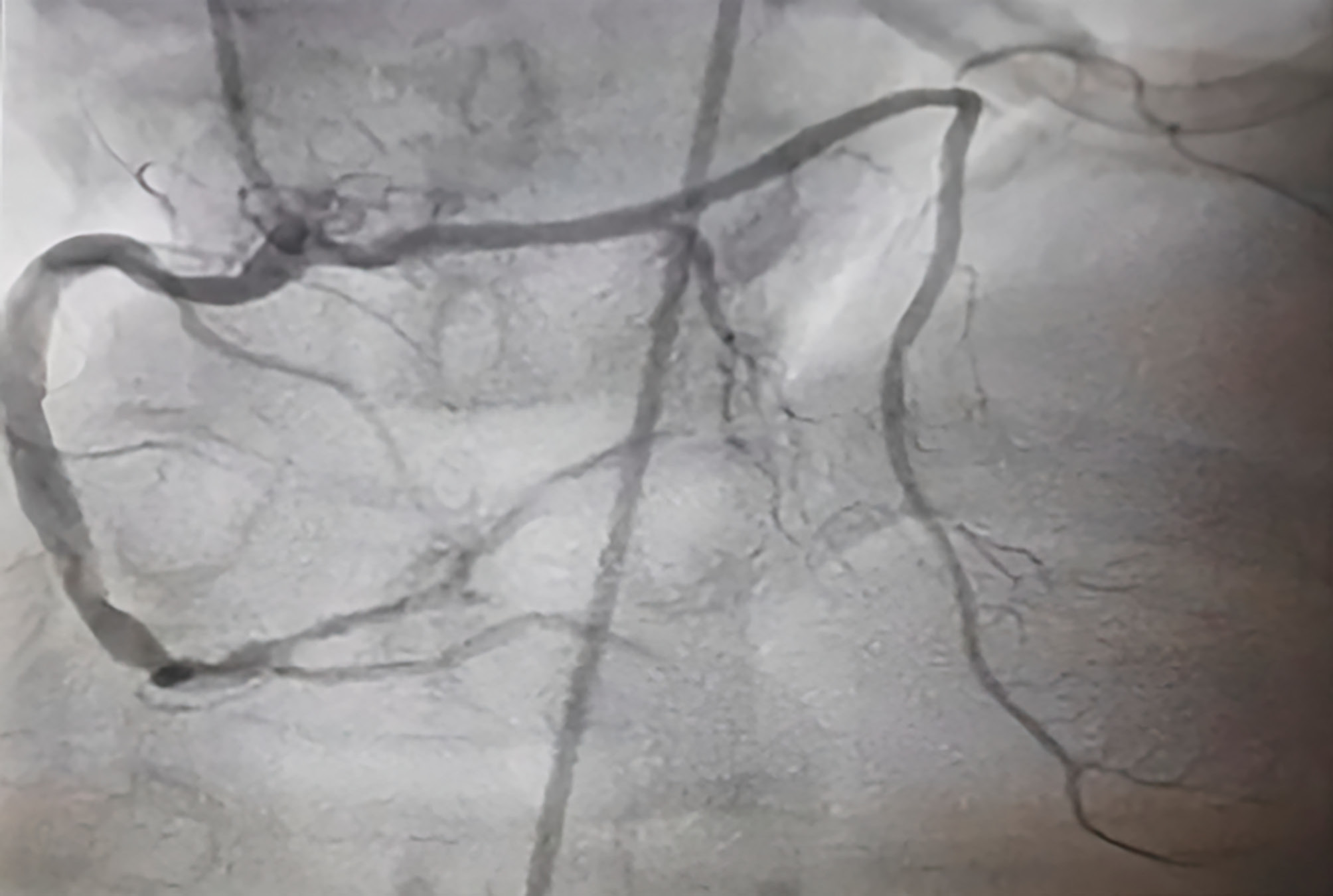
Figure 1. Right anterior oblique cranial projection of the right coronary artery (RCA) showing a second left anterior descending artery (LAD) arising from the proximal RCA and leading to the anterior interventricular septum, with septal branches and a totally occluded third diagonal branch.
Conflict of interest statement
The authors have no conflicts of interest to declare, and there has been no financial support for this work that could influence its findings.