Blood flow through an aneurysmal or ectatic segment of a coronary artery is often sluggish because of the formation of eddy currents, leading to thrombogenesis in these regions1. We report on a patient where the altered flow in an ectatic artery with a focal aneurysm masqueraded as a thrombus.
A 52-year-old male smoker presented with inferior wall myocardial infarction. His workup was negative for any current or prior infection and connective tissue disorders. Angiography revealed a large, dominant, ectatic left circumflex artery (LCx) with a filling defect in the proximal segment (Figure 1A, Moving image 1) and thrombotic occlusion of the left posterior descending artery (LPDA). We deduced that the proximal thrombus had embolised distally, and hence, we planned for thrombus aspiration. After wiring the vessel, multiple aspiration runs were performed, at both the proximal ectatic portion and the distal occluded vessel, and there was restoration of flow beyond the distal occlusion, revealing a tight lesion. However, the filling defect at the proximal ectatic portion persisted (Figure 1B, Moving image 2) after the correction had been done. An intravascular ultrasound examination of the ectatic segment was performed, which intriguingly revealed no intraluminal thrombus (Figure 1D and Figure 1E, top marked with *). Chromaflo imaging confirmed that there was no filling defect; however, there seemed to be decreased flow velocities at the aneurysmal segment (Figure 1D and Figure 1E, top marked with $). The LPDA origin had a significant lesion (Figure 1C); this was successfully stented. Selective intubation of the LCx with the guiding catheter and angiogram, using a larger contrast volume (approximately 10 ml) and faster injection, showed no filling defect in the focal aneurysm (Figure 1E, Moving image 3).
When the contrast volume during angiography is insufficient to fill the entire vessel, it may fail to displace the blood present in an eccentric aneurysm, making it appear as a filling defect (flow void). This is possibly due to lack of contact between the outermost fluid envelope and the aneurysmal segment (Figure 1F). Intravascular imaging can help us understand this better and can avoid stenting an aneurysmal segment, which is both technically challenging and has been shown to have poorer outcomes1. Coronary artery aneurysms also tend to have increased incidence of thrombus1, hence in our case, we discharged our patient with a plan of 3 months of triple anticoagulation, followed by a plan to continue single antiplatelet therapy with oral anticoagulation.
To the best of our knowledge, this is the first description of flow void in coronary artery stenosis angiographically masquerading as a thrombus. One must be mindful of this entity especially when dealing with a diffusely ectatic vessel with a focal aneurysm.
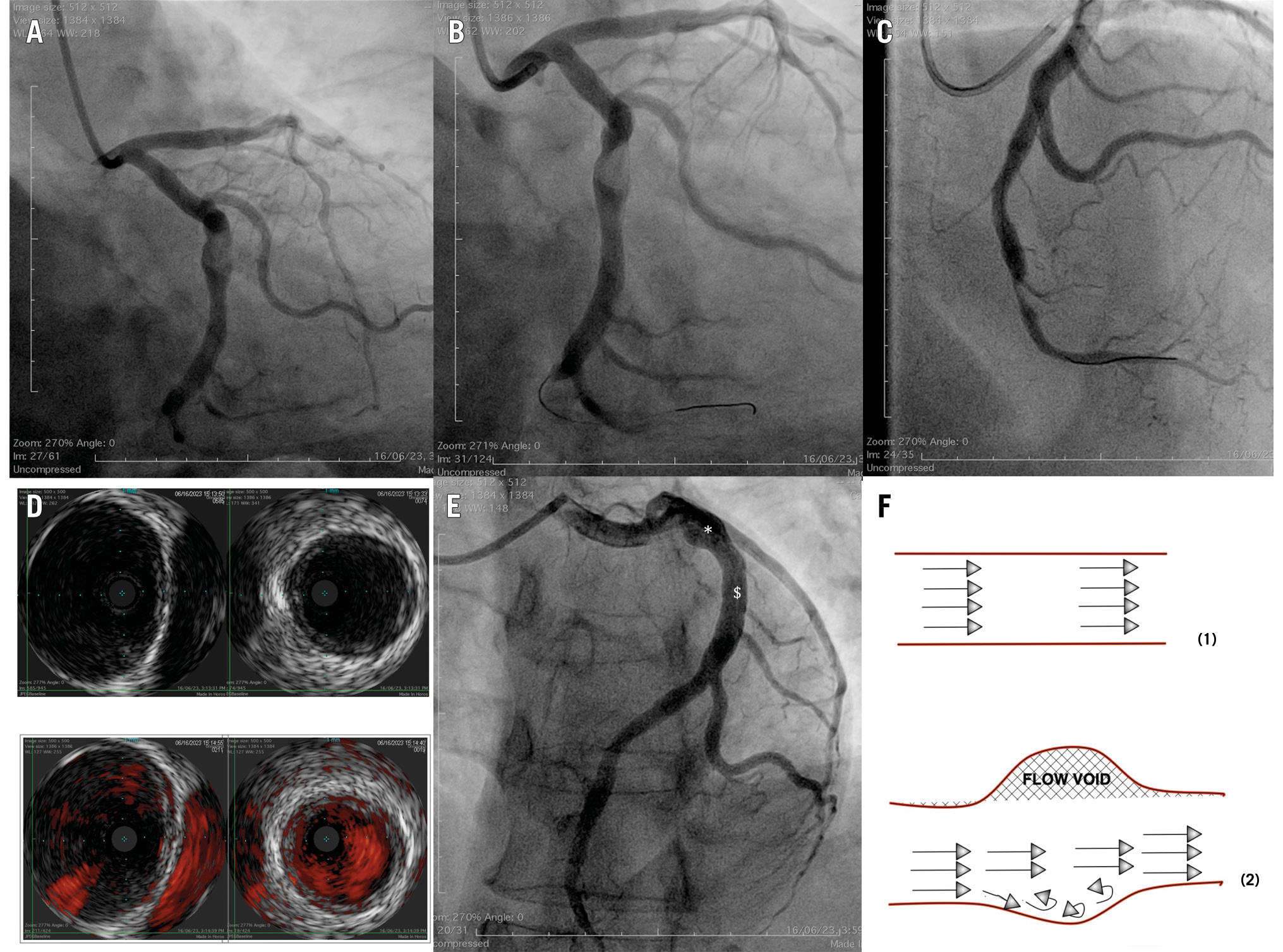
Figure 1. Imaging sequence showing flow void. A) Proximal LCx filling defect. B) Persisting filling defect after repeated thrombosuction. C) Stenotic lesion at origin of LPDA. D) IVUS of a focal aneurysm with no filling defect; reference distal LCx (top); Chromaflo (bottom). E) Cineangiography with no filling defect; DES to LPDA. F) Blood flow: (1) normal flow; (2) inadequate flow through an ectatic vessel. DES: drug-eluting stent; IVUS: intravascular ultrasound; LCx: left circumflex artery; LPDA: left posterior descending artery
Conflict of interest statement
The authors have no conflicts of interest to declare.
