Successful guidewire passage through the main vessel (MV) and side branch (SB) is the key to successful percutaneous coronary interventions (PCI) of bifurcation lesions. Even if provisional stenting is considered, SB wiring is routine in interventional practice. It can sometimes be challenging to wire the distal main branch (DMB) or SB in certain complex bifurcation lesions, requiring a specific technique or hardware. In general, it is the SB access which is troublesome to secure in difficult bifurcation lesions; occasionally, DMB access may be difficult in comparison to SB access. The common reasons for such difficult access are significant calcification/stenosis, large eccentric plaque burden and tortuosity of the proximal MV, which limit guidewire manipulations across the bifurcation site1. An angulation between the main axis of the MV and the main axis of the DMB/SB is also crucial for successful wiring. Often the branch at a wider angulation from the MV axis is the one where difficult wiring occurs. Wiring is difficult with an angle of >70°2. Conventionally, different types of wires and their tip curvatures along with proximal MV plaque modification help in DMB/SB access3. We hereby report our experience of difficult DMB access in bifurcation lesions, for which an SB balloon block and support technique was used for successful DMB wiring, during the PCI. We retrospectively analysed our PCI data from June 2007 to January 2018 and found 6 eligible patients from 4,712 PCI performed during this period. All these cases had unsuccessful DMB wiring using the conventional method. As there was a significant plaque burden at the bifurcation carina and the proximal MV axis was favouring the SB, the guidewire tip kept slipping into the SB and missing the DMB entry. Multiple attempts were made by using different wire and tip configurations, such as a single bend with a short or long tip, single wide bend and double bend, to cross the DMB. Plaque modification of the proximal MV to avoid the risk of DMB occlusion was not considered in any of the patients. After multiple unsuccessful attempts to wire the DMB, we came up with an unorthodox approach. Following the wiring of the SB, an undersized semi-compliant balloon (balloon to SB diameter ratio <1.0) was positioned at the SB, 1-2 mm distal to the bifurcation carina. Another coronary guidewire with a single wide bend or double bend tip (Figure 1) was advanced and positioned at the proximal MV, near the carina. Thereafter, the SB balloon was inflated at low pressure (7-8 atms) to block the flow across the SB, which was confirmed by the contrast injection. Then, attempts were made to negotiate the wire to the DMB with the support of an inflated SB balloon. The inflated SB balloon helped to direct the wire into the DMB instead of it slipping into the SB. The duration of the SB balloon occlusion during each attempt was less than 45 seconds, to avoid ischaemia of the SB-supplied territory. Following the successful wiring of the DMB, the balloon was deflated and removed from the SB, and the standard PCI procedure was completed. All PCI procedures were performed following the acquisition of written informed consent. The study protocol for retrospective analysis of the cases was approved by the institute’s ethics committee. The mean age of the 6 patients was 60±11.69 years. There were 5 males and 1 female. The clinical diagnosis was acute myocardial infarction in 2 patients, unstable angina in 3 patients and chronic stable angina in 1 patient. Three patients had bifurcation lesions in the left anterior descending/diagonal branch (Figure 2), two in the left circumflex/obtuse marginal branch (Figure 3, Figure 4) and one in the right coronary artery/right ventricle branch (Figure 5). The bifurcation lesion morphology was Medina 1,1,0 in three cases, 1,1,1 in two cases, and 0,1,0 in one case. The mean bifurcation angle was 70±8.6° (range 60°-90°). In all cases, a hydrophilic wire was preferred to cross the DMB. A BMW wire (Abbott), a SION blue wire (Asahi Intecc) and a Persuader 3 wire (Medtronic) were used in one case each, while a Choice PT wire (Boston Scientific) was used in the remaining 3 cases. The number of times the SB balloon was inflated for DMB successful wiring varied from 2-6 times. Table 1 describes the patient and lesion characteristics and procedural details. The SB remained patent with Thrombolysis in Myocardial Infarction (TIMI) grade 3 flow in all cases following provisional MV stenting. All patients were asymptomatic at a median of 51 months of clinical follow-up.
The traditional techniques for DMB wiring include reshaping of the guidewire’s tip, wire pullback technique and reverse wire technique4. Another approach to wire these lesions is upstream plaque debulking or modification before DMB wiring, which has an inherent risk of DMB occlusion4. There are certain devices, such as a deflectable tip venture catheter or double-lumen microcatheter, which are useful but have additional costs for the procedure56. Appropriate wire tip shaping is the first and preferred method to cross a lesion. A single bend with a short tip is preferable in cases with narrow bifurcation angles, while a wide smooth bend is better suited to cross lesions with wider bifurcation angles. A wide double bend is helpful in wide bifurcation angles, especially when the SB ostium has a critical disease3. Using these routine manoeuvres, there is a possibility of failing to cross the lesions, as experienced in the present study. The SB balloon block and support technique is not described in the published literature. However, Li et al published a similar procedure where an MB balloon block and support technique was used to wire a difficult SB7. With the SB balloon block and support technique, there are certain complications such as ischaemia of the SB territory due to repeated and prolonged balloon inflation and SB dissection/occlusion; however, we did not experience any such complications. As hydrophilic guidewires are more slippery and, increasingly, trackable with reduced friction, they were used in all cases. Though we achieved successful DMB wiring in all patients, the technique might be unsuccessful and associated with certain complications such as dissection or occlusion of the DMB/SB. Our study has the inherent limitations of a retrospective analysis of a small sample size and an experience from a single centre. In conclusion, the use of an SB balloon block and support technique allowed for a successful guidewire crossing of the DMB, where conventional methods had failed, in a series of six patients undergoing PCI.
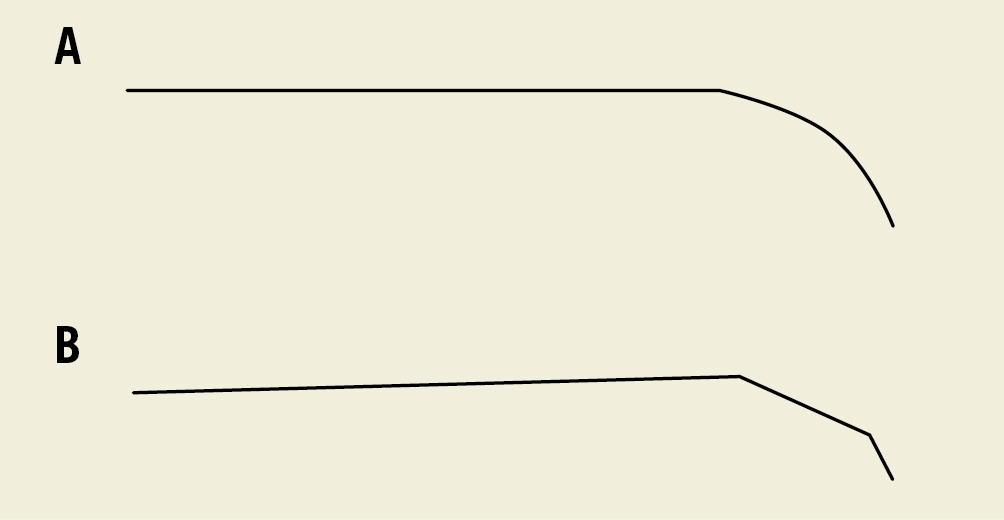
Figure 1. Shape of coronary guidewire tip to facilitate distal main branch entry. Guidewire tip shape as wide smooth bend (A) and double bend (B) to wire the distal main branch.
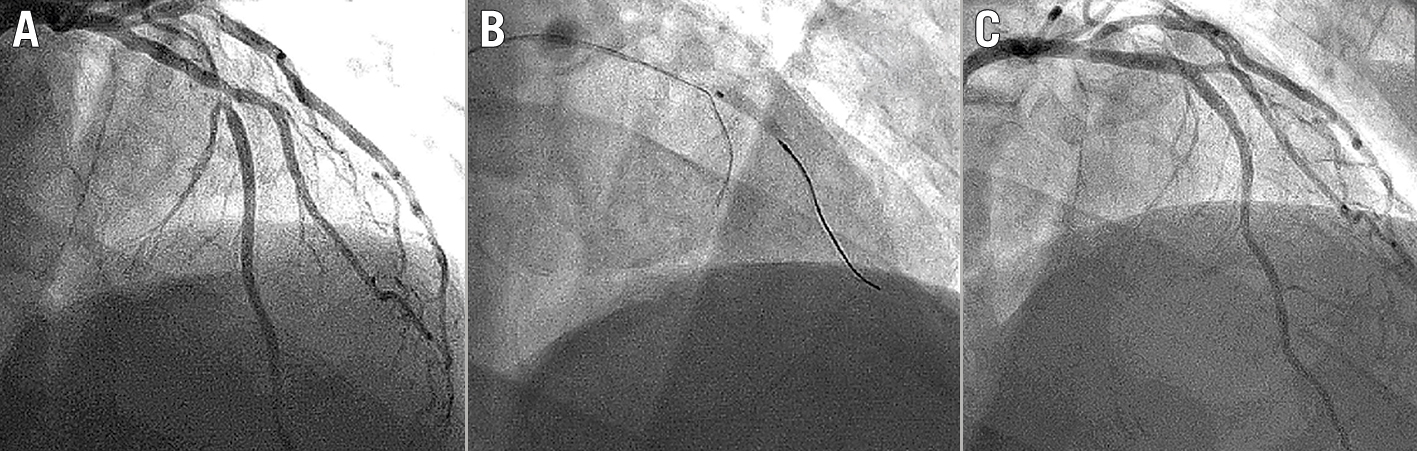
Figure 2. Percutaneous coronary intervention of a left anterior descending/diagonal bifurcation lesion. Coronary angiogram showed mid-left anterior descending (LAD)/diagonal (D1) bifurcation stenosis (Medina 0,1,0) (A). A 2.5 mm balloon was inflated at the D1 ostium, to direct the wire crossing to the distal LAD (B). TIMI 3 flow was achieved in LAD/D1 following LAD stenting (C). (Case 3 of Table 1)

Figure 3. Percutaneous coronary intervention of a bifurcation lesion of the obtuse marginal branch. Coronary angiogram showed bifurcation stenosis of the obtuse marginal branch (OM1) (Medina 1,1,0) (A). A 2.25 mm balloon was inflated at the ostium of the first side branch of OM1 (B) to direct the wire crossing to the distal OM1 (C). TIMI 3 flow was achieved in OM1 following stenting (D). (Case 2 of Table 1)
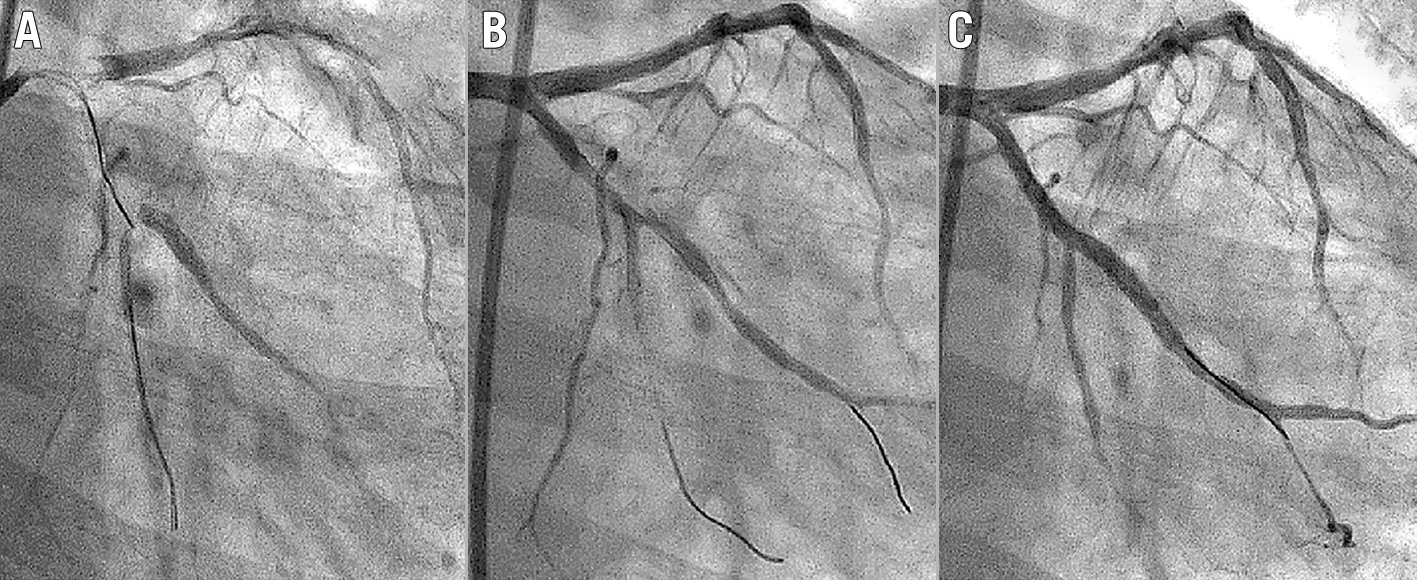
Figure 4. Percutaneous coronary intervention of a left circumflex/obtuse marginal bifurcation lesion. Coronary angiogram showed proximal left circumflex (LCx)/obtuse marginal (OM1) bifurcation stenosis (Medina 1,1,1) (A). A deflated balloon was present in the distal LCx following successful wire crossing of OM1 (B). There was wire-induced dissection of OM1 (B). TIMI 3 flow was achieved in LCx/OM1 following LCx-OM1 stenting (C). (Case 6 of Table 1)
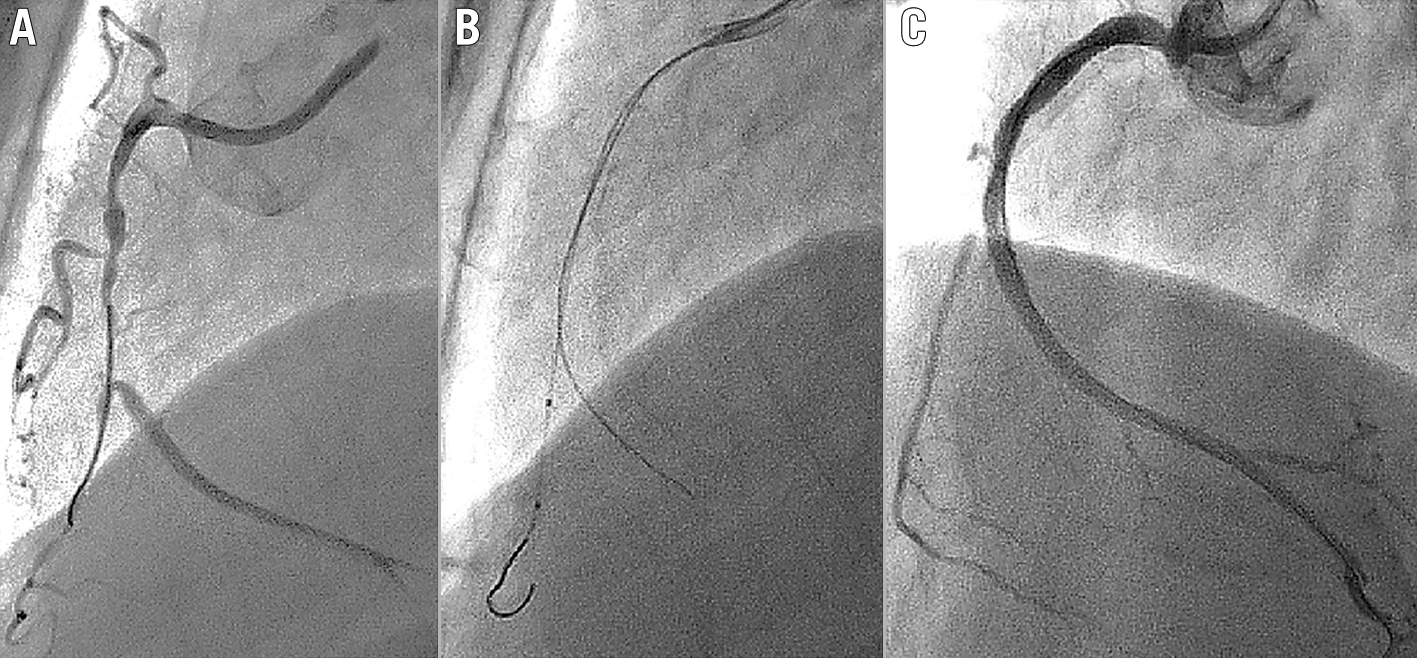
Figure 5. Percutaneous coronary intervention of a right coronary artery/right ventricle bifurcation lesion. Coronary angiogram of right coronary artery (RCA) showed bifurcation stenosis of the mid-RCA/right ventricle (RV) branch (Medina 1,1,1) (A). A deflated balloon was present in the RV branch following successful wiring of the mid-RCA (B). TIMI 3 flow was achieved in the RCA following stenting (C). (Case 1 of Table 1)
Table 1. Clinical and procedural details of 6 patients.
| Case no. | Age (years) /sex | Diagnosis | Bifurcation lesion site | Medina classification | Bifurcation angle (°) | No. of times balloon was inflated | Side branch’s balloon diameter (mm) |
|---|---|---|---|---|---|---|---|
| 1 | 40/M | AMI | RCA/RV branch | 1,1,0 | 61 | 3 | 3 |
| 2 | 75/M | USA | OM main and side branch | 1,1,0 | 87 | 2 | 2.25 |
| 3 | 68/M | USA | Mid-LAD/D2 | 0,1,0 | 65 | 2 | 2.5 |
| 4 | 59/F | AMI | Mid-LAD/D2 | 1,1,0 | 64 | 3 | 2.5 |
| 5 | 67/M | CSA | Mid-LAD/D3 | 1,1,1 | 74 | 6 | 2 |
| 6 | 51/M | USA | LCx/OM | 1,1,1 | 69 | 4 | 2 |
| AMI: acute myocardial infarction; CSA: chronic stable angina; D: diagonal; LAD: left anterior descending; LCx: left circumflex; OM: obtuse marginal; RCA: right coronary artery; RV: right ventricle; USA: unstable angina | |||||||
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest statement
The authors have no conflicts of interest to declare.

