Introduction
Imaging with 18F-Fluorodeoxyglucose positron emission tomography/computed tomography (18F–FDG PET/CT) plays an important role in the diagnosis of cardiovascular infection and inflammation. Current European Society of Cardiology guidelines include abnormal periprosthetic uptake in 18F–FDG PET/CT as a major criterion in the diagnosis of infective endocarditis if performed >3 months after surgical valve implantation1. While the characteristics of 18F–FDG PET/CT uptake in noninfected patients with surgically implanted prosthetic aortic valves have been described2, data on 18F–FDG PET/CT uptake following transcatheter aortic valve replacement (TAVR) are limited345. Importantly, the pattern of 18F–FDG PET/CT uptake immediately following TAVR, which represents the inflammatory response to injury, is unknown.
Methods
We performed a prospective analysis of 18F–FDG PET/CT uptake in patients who underwent a TAVR procedure over an 8-month study period at our institution. Patients with fever, elevated white cell count, erythrocyte sedimentation rate, high-sensitivity C-reactive protein, or positive blood or urine cultures preprocedure were excluded. The study was approved by the ethics committee of the Ministry of Health, Kuwait. Continuous variables were expressed as mean±standard deviation, and categorical variables were expressed as numbers or percentages.
Results
A total of 17 consecutive patients were studied (female 53%, age 72.6±7.3 years, diabetes mellitus 76.5%, hypertension 94.1%, history of myocardial infarction 11.8%, history of coronary artery bypass surgery 11.8%). TAVR was performed using balloon-expandable (SAPIEN 3 [Edwards Lifesciences], n=8) or self-expanding (Evolut R [Medtronic], n=9) devices. 18F–FDG PET/CT was performed in all patients within 7 days of TAVR. Briefly, patients were prescribed a high-fat and low-carbohydrate diet for 72 hours before the study, with a minimum fasting period of 12 hours. Heparin 50 IU/kg was administered intravenously 15 minutes before the radiotracer. Patients received 0.06 mCi/kg of 18F-FDG intravenously and images were obtained after 60 minutes (early) and 120 minutes (late). The maximum standard uptake value (SUVmax) was obtained from the implant site and from the liver as reference. The SUVratio was obtained by dividing the SUVmax of the implant site by the SUVmax of the liver. Valvular uptake patterns were analysed from axial views and classified as circumferential (>75% of valvular circumference), hemicircumferential (25% to 75% of valvular circumference), focal (<25% of valvular circumference), or multifocal (≥2 focal uptakes).
18F–FDG PET/CT demonstrated positive periprosthetic uptake in all patients. The uptake patterns were hemicircumferential (n=12) and circumferential (n=5) (Figure 1); a focal pattern was not seen in any of the patients. There were no differences in the uptake pattern or SUVratio (1.05±0.22 versus 1.04±0.07; p=0.9) between the Evolut R and SAPIEN 3 implants. High-sensitivity C-reactive protein was elevated in all patients post-TAVR (all these patients had normal levels at baseline before the TAVR procedure), with no significant difference between the uptake patterns (hemicircumferential 71.3±69.6 mg/L vs circumferential 47.06±22.4 mg/L; p=0.5). Erythrocyte sedimentation rates and white cell counts were not elevated post-TAVR. One patient required a permanent pacemaker insertion post-TAVR.
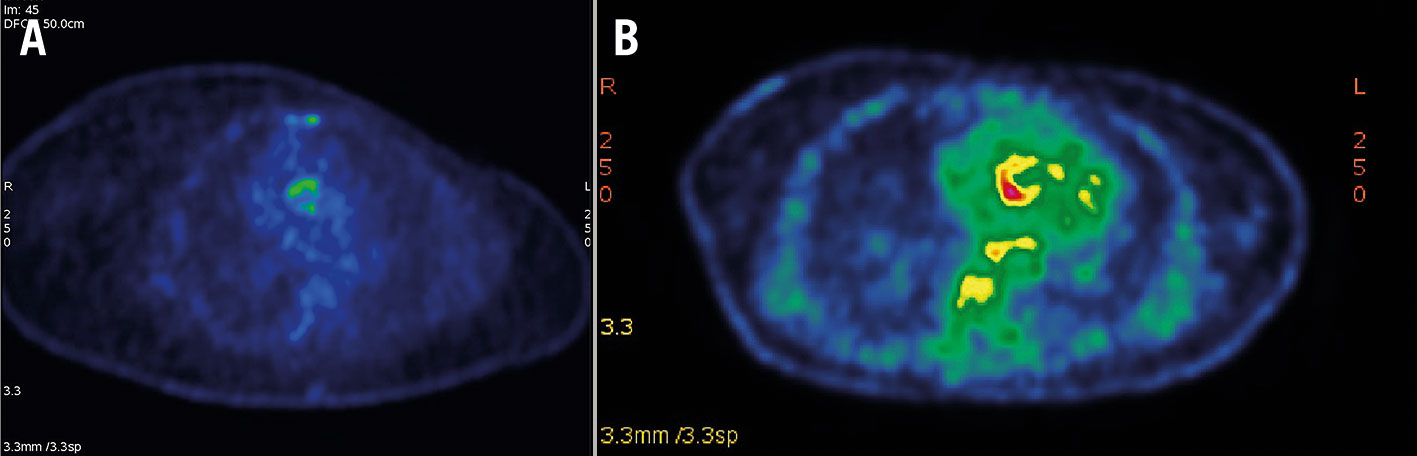
Figure 1. Representative images of 18F-fluorodeoxyglucose uptake patterns. A) Hemicircumferential and B) circumferential positive uptake after TAVR. TAVR: transcatheter aortic valve replacement
Discussion
We describe for the first time the pattern of acute 18F–FDG PET/CT uptake following TAVR, representing solely the inflammatory response to the procedure without the confounding effect of a coexisting infection. Available data on 18F–FDG PET/CT uptake patterns following TAVR are limited and rather varied. For instance, del Val et al concluded that noninfected patients do not exhibit significant periprosthetic 18F–FDG PET/CT uptake 3 months after TAVR and have suggested that significant periprosthetic uptake >3 months after TAVR may be highly indicative of infective endocarditis3. On the other hand, 23% of noninfected patients demonstrated positive periprosthetic uptake of 18F–FDG PET/CT at 1 month and 13% at 3 months post-TAVR in another study4. San et al have also suggested that uptake patterns could be used to accurately differentiate between noninfected patients and patients with infective endocarditis; the 18F–FDG PET/CT uptake pattern was hemicircumferential or circumferential in noninfected patients, and focal or multifocal in patients with infective endocarditis in their study4. However, contrary to the study by San et al, a hemicircumferential uptake was demonstrable in patients with infective endocarditis at 3 months, and even as late as 8 months, after TAVR in a study by Salaun et al5. Our study findings indicate that the focal/multifocal 18F-FDG uptake pattern that has been described in patients with infective endocarditis4 is not seen in noninfected patients in the 7 days following TAVR. Therefore, the presence of a focal/multifocal 18F-FDG uptake pattern within the 7 days following TAVR could raise the suspicion of infective endocarditis in some patients who may develop a high-grade fever (≥38.0oC) following the procedure.
With regard to the mechanisms underlying the differing patterns of circumferential and hemicircumferential uptake in noninfected post-TAVR patients, we would like to speculate that these could be related to the differences in response to injury in different patients, the underlying mechanisms of which are yet to be determined. In our study, all TAVR devices were slightly oversized according to current recommendations, and the degree of oversizing was similar among the patients. Post-implantation balloon aortic valvuloplasty was required in only 3 patients (all of whom had self-expanding devices, including 1 patient who also required predilatation). Hence, it is difficult to determine if pre/post-balloon dilatation would have contributed to different patterns of FDG uptake.
Although quantification of valvular calcification by CT prior to TAVR was not part of the study design, we observed that 18F–FDG PET/CT uptake patterns did not correspond to the distribution of valvular calcification assessed by pre-TAVR CT, and an intense inflammatory response was also seen in areas without underlying calcification. This observation is interesting, as it may lead to speculation that the local inflammatory response following TAVR is likely to result from soft tissue injury.
Limitations
Limitations of this study include a small sample size and the absence of serial imaging; thus, it might be difficult to obtain long-term results. It is anticipated that these uptake patterns are likely to change with time, and their evaluation may require serial imaging studies which were not part of the study design.
Conclusions
Our study, which describes the pattern of acute periprosthetic uptake of 18F–FDG PET/CT in patients following TAVR, demonstrated a positive uptake in all patients and represents the inflammatory response to injury assessed non-invasively following implantation. The pattern of uptake was distinctively hemicircumferential or circumferential, with an absence of focal/multifocal patterns. Larger studies with serial imaging are needed to evaluate patterns of 18F–FDG PET/CT uptake at baseline, immediately post-TAVR, and at specific timepoints from the index procedure, and to compare with patients with infective endocarditis. Because 18F–FDG PET/CT imaging can non-invasively describe the extent of inflammation due to injury following TAVR both anatomically and metabolically, it would be interesting to evaluate its role in predicting long-term outcomes such as structural valve deterioration.
Conflict of interest statement
The authors have no conflicts of interest to declare.
