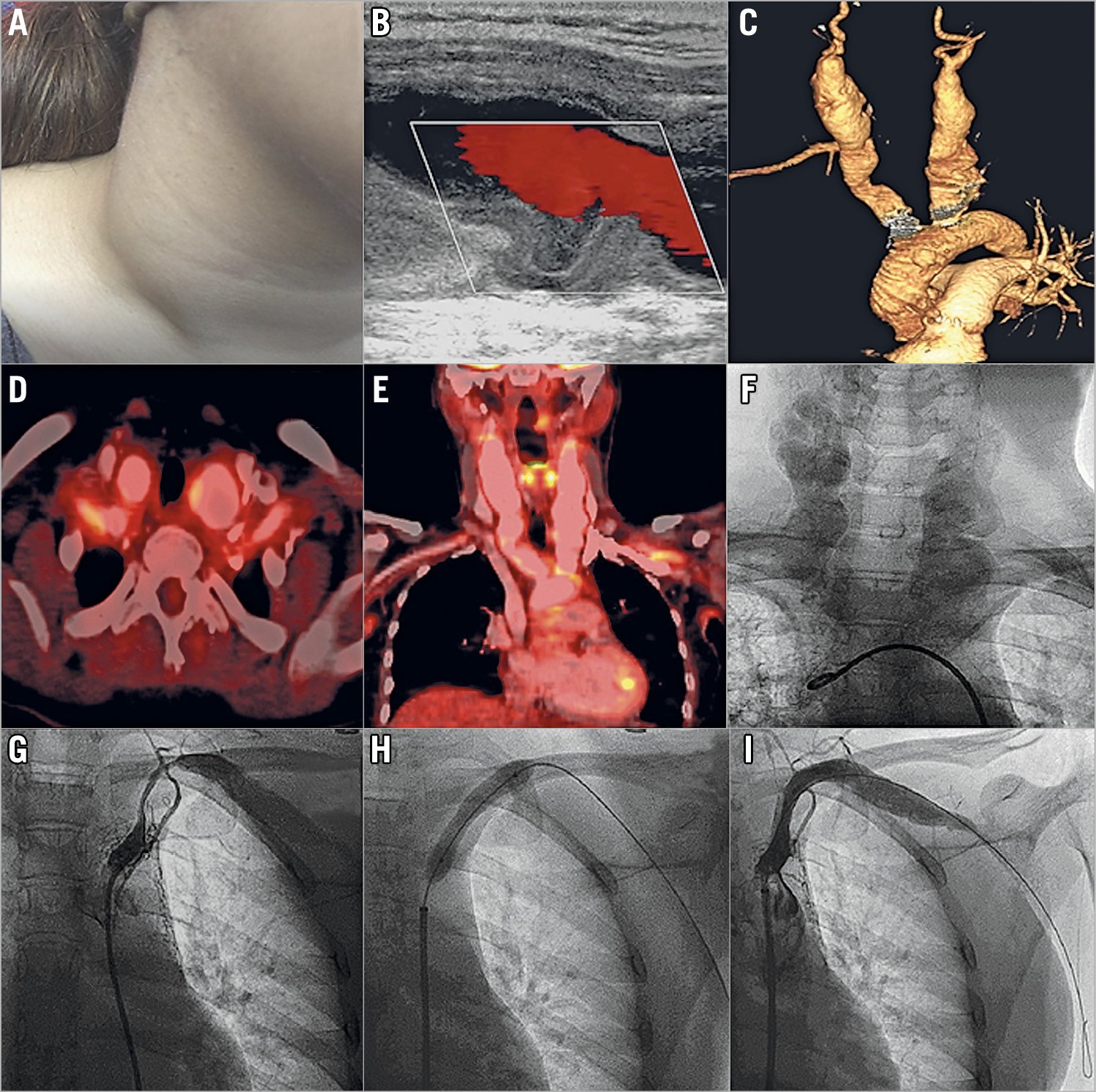
A 20-year-old girl presented with a history of low-grade fever and weight loss for the previous six months and disabling rest pain of the left upper limb for the last one month. She had also observed bilateral pulsatile swelling of the neck for the last three weeks. Systemic examination revealed a diminished left radial pulse and bilateral 3×3 cm expansile pulsating mass in the neck (Panel A, Moving image 1). The systolic blood pressure of the right and left upper limb was 100 and 60 mmHg, respectively. Doppler ultrasound revealed a bilateral common carotid artery (CCA) aneurysm with intraluminal spontaneous swirling contrast (Panel B, Moving image 2). Computed tomography angiography revealed diffuse, circumferential mural thickening of the bilateral subclavian artery (SCA) and a fusiform aneurysm of the bilateral CCA, the right brachiocephalic artery extending from the aortic ostium to the extra-cranial, carotid bifurcation site (Panel C). Additionally, the left SCA had 90% proximal stenosis. Her erythrocyte sedimentation rate and plasma C-reactive protein were raised. 18F-fluorodeoxyglucose positron emission tomography showed increased uptake in the aortic arch, and its branches consistent with active, large vessel vasculitis (Panel D, Panel E). She was treated with oral prednisolone 1 mg/kg and methotrexate 15 mg/week for active Takayasu’s arteritis. After a month of therapy, she had improved constitutional symptoms, appetite and body weight. A contrast angiogram confirmed a bilateral CCA fusiform aneurysm and 90% stenosis of the left SCA (Panel F, Panel G, Moving image 3). Following balloon angioplasty with an 8×40 mm balloon, there was a brisk flow across the SCA (Panel H, Panel I). She was later referred for open surgical revascularisation of bilateral CCA aneurysms.
Conflict of interest statement
The authors have no conflicts of interest to declare.

