Rajiv Ananthakrishna1,2, DM; Adrian F. Low1*, MBBS
AsiaIntervention 2019;5:128-129, DOI: 10.4244/AIJ-D-19-00003
1. Department of Cardiology, National University Heart Centre, Singapore; 2. Department of Cardiology, Sri Jayadeva Institute of Cardiovascular Sciences and Research, Bangalore, India
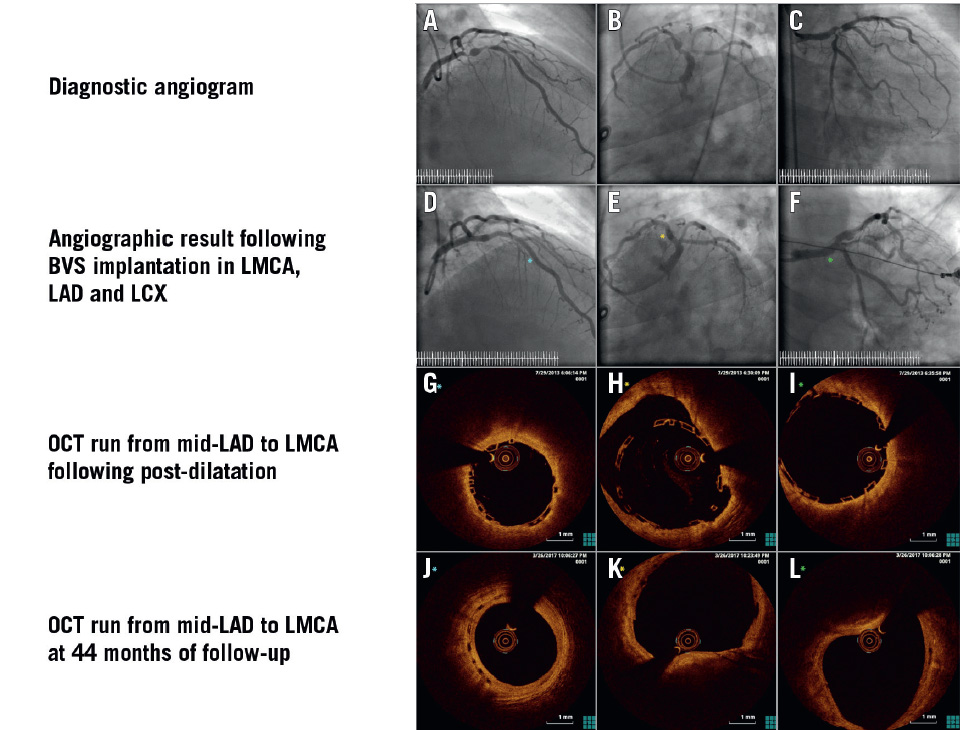
A 54-year-old male underwent coronary angiography for non- ST-elevation myocardial infarction. This identified significant proximal left anterior descending artery (LAD) disease with an aneurysm (Panel A). In addition, the ostial left circumflex (LCX) and first obtuse marginal (OM1) had significant disease (Panel B, Panel C). The OM1 lesion was treated with a 3.0×26 mm SeQuent® Please (B. Braun, Melsungen, Germany) drug-eluting balloon. A 3.0×18 mm Absorb™ bioresorbable vascular scaffold (BVS) (Abbott Vascular, Santa Clara, CA, USA) was implanted from the ostial LCX. Subsequently, two additional Absorb BVS were implanted from the distal left main coronary artery (LMCA) to the proximal LAD (3.5×28 mm), and the mid-LAD (3.0×18 mm). The final angiographic result is shown in Panel D-Panel F. An optical coherence tomography (OCT) study from the mid-LAD to the LMCA showed well expanded struts without scaffold fracture (Panel G-Panel I, Moving image 1, Moving image 2). The scaffold was malapposed in the aneurysmal segment (Panel H, Moving image 2, Moving image 3). The minimal luminal area (MLA) measured 8.13 mm2 in the LAD and 12.87 mm2 in the LMCA at the end of the procedure (Moving image 3). The patient was on dual antiplatelet therapy (aspirin and clopidogrel) for 30 months, followed by single antiplatelet therapy with aspirin.
There are concerns following the implantation of BVS, with reports of early as well as late scaffold failure, resulting in adverse cardiac outcomes. As this was a complex lesion subset, we performed a repeat angiogram with OCT at 44 months to ensure that there were no complications related to BVS implantation. The coronary angiogram showed a patent LMCA, LAD, LCX and OM1 (Moving image 4-Moving image 6). An OCT study was performed from the mid-LAD to the LMCA. The majority of the strut remnants showed complete endothelialisation with positive remodelling (Panel J-Panel L, Moving image 7, Moving image 8), including the aneurysmal segment (Panel K, Moving image 8). The MLA measured 12.35 mm2 in the LAD and 15.79 mm2 in the LMCA at matched cross-sections (Moving image 8).
Long-term follow-up concerning BVS deployment in lesions with coronary aneurysm is lacking. On the other hand, coronary aneurysm formation is a well described complication following implantation of drug-eluting stents and BVS. In addition, this complication has also been described with novolimus-eluting BVS. Hence, the implantation of a scaffold to an aneurysmal lesion with long-term OCT follow-up demonstrating resorption is unique in this patient. The risk of scaffold thrombosis in the aneurysmal segment persists until the struts are completely resorbed. There are no protective factors for scaffold thrombosis in the initial period following implantation. At 44-month follow-up, OCT showed completely endothelialised strut remnants in the aneurysmal segment. Therefore, complete resorption in the aneurysmal segment results in the absence of late strut malapposition, and probably a lower risk of very late scaffold thrombosis.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. OCT run from mid-LAD to proximal LAD during the index procedure.
Moving images 4. Coronary angiogram at 44-month follow-up.
Moving images 5. Coronary angiogram at 44-month follow-up.
Moving images 6. Coronary angiogram at 44-month follow-up.
Moving image 7. OCT run from mid-LAD to LMCA at 44-month follow-up.
Moving image 8. 3D OCT run from proximal LAD to LMCA at 44-month follow-up.
To download, please click below.