Introduction
Mitral regurgitation (MR) is a common form of valvular heart disease affecting 2-12% of the general population, and is the second most common valvular indication for cardiac surgery1,2,3,4. The aetiology of MR is conventionally divided into primary, as a disease affecting valve leaflets, or secondary, with pathology of the mitral valve apparatus and/or left ventricle excluding valve leaflets1,2. This classification is important in the prognosis, which is worse for secondary MR, and in the determination of management strategy6,7. Mitral valve surgery (MVS) is the established gold standard method for treating severe primary MR with symptoms, impaired left ventricular ejection fraction, dilated left ventricular end-systolic diameter, new onset atrial fibrillation or severe pulmonary hypertension, and surgical repair is preferable to replacement where feasible1,2. The efficacy of MVS in treating primary MR has not translated to the treatment of secondary MR, where management remains controversial, creating an unmet need in these and other high-risk candidates with severe MR8,9.
Minimally invasive procedures for valvular heart disease have blossomed over the last decade, and for MR, the percutaneous MitraClip™ (Abbott Vascular, Santa Clara, CA, USA) procedure was the first readily available technology10. EVEREST-II was the first randomised trial comparing the MitraClip procedure to MVS for primary MR11. Two further trials explored the MitraClip procedure compared to medical therapy for secondary MR with conflicting results12,13. Nevertheless there remains limited randomised evidence for the MitraClip procedure and its exact role and indications remain controversial. This meta-analysis compared the efficacy and safety outcomes of the MitraClip procedure with MVS in patients with severe MR.
Methods
LITERATURE SEARCH
The meta-analysis was conducted in accordance to the PRISMA guidelines. Relevant studies and abstracts, from January 1, 1980 to June 30, 2019, were identified through searching five electronic databases including Medline, Embase, PubMed, Cochrane Central Register for Controlled Trials (CENTRAL), and Scopus. The search terms used were “MitraClip”, “percutaneous”, “transcatheter”, “catheter-based”, or “endovascular”; AND “mitral regurgitation”. The reference lists of retrieved articles were then screened for potentially relevant studies. Two reviewers (TW and MW) independently conducted the search and evaluated studies for inclusion. Differences were resolved by discussion and consensus.
INCLUSION AND EXCLUSION CRITERIA
Original studies comparing the MitraClip procedure and mitral valve surgery outcomes in more than twenty adult human subjects (over 18 years of age) with significant mitral regurgitation were eligible for inclusion. Mortality outcomes for both the MitraClip procedure and MVS had to be reported. Both randomised trials and observational studies were included, and reviews were excluded. When multiple publications reported results from the same trial or cohort, data were extracted and pooled as one study.
DATA EXTRACTION
Three reviewers (TW, AC and MW) independently extracted data, using standardised forms. Differences were resolved by discussion and consensus. Data were extracted on study design, patient and intervention characteristics, and both short- and long-term mortality and morbidity outcome measures.
STATISTICAL ANALYSIS
Statistical analyses were performed using Review Manager Version 5.3 (Cochrane Collaboration, Oxford, UK). Variables reported by two or more studies were pooled. Meta-analyses were conducted using odds ratios (OR) or weighted mean differences (WMD) with 95% confidence intervals (95%CI), some presented as forest plots. Random effects modelling was utilised to account for potential variation in methodology and participant characteristics between studies. Heterogeneity of studies and publication bias were assessed using the I² test and funnel plots for each outcome pooled, and no significant heterogeneity or evidence of publication bias were found for any outcomes. All tests were two-tailed and p<0.05 was considered significant.
Results
There were 959 articles identified from the literature search. Following abstract review and exclusion of 938 unrelated or duplicate articles, the 21 full-text articles were evaluated. Six of these studies did not report both treatment modalities of interest, and six were duplicate trials, leaving nine studies meeting the inclusion criteria selected for subsequent analysis11,14,15,16,17,18,19,20,21,22. The study design of included studies is summarised in Table 1. There was one randomised trial and eight retrospective observational cohort studies, totalling 1,171 patients (640 MitraClip procedures and 531 MVS), followed-up for 6-60 months.
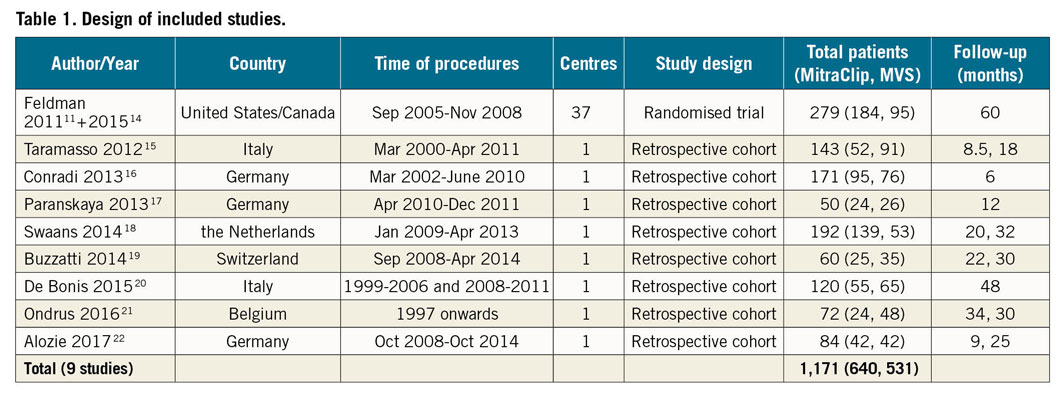
Patient characteristics for both treatment arms of these studies are shown in Table 2. In the MVS arm, 485 (91%) were mitral valve repairs. MitraClip patients were older, had higher proportion of previous cardiac surgery, coronary artery disease, and logistic EuroSCORE 1, while the proportion of males, patients with New York Heart Association (NYHA) classification III-IV, functional MR and left ventricular ejection fraction (LVEF) ranges were similar between the two arms.
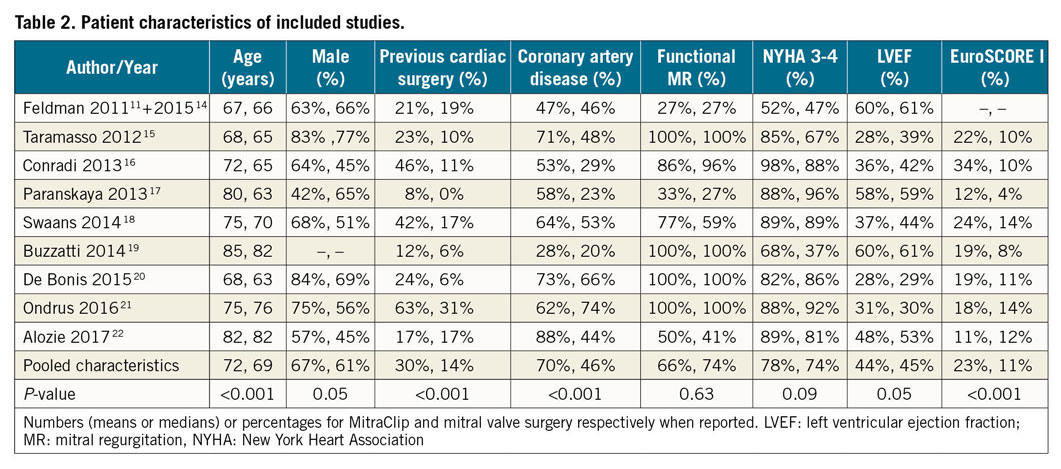
Figure 1 illustrates the forest plots for pooled mortality outcomes. There were no statistically significant differences between the MitraClip procedure and MVS for operative mortality, 3% versus 5% (OR: 0.58, 95% CI: 0.28-1.19, p=0.14) overall in eight studies; one-year mortality 12% versus 13% (OR: 1.09, 95% CI: 0.71-1.68, p=0.69) in seven studies; and long-term mortality 30% versus 35% (OR: 0.99, 95% CI: 0.69-1.4, p=0.97) in four studies, respectively.
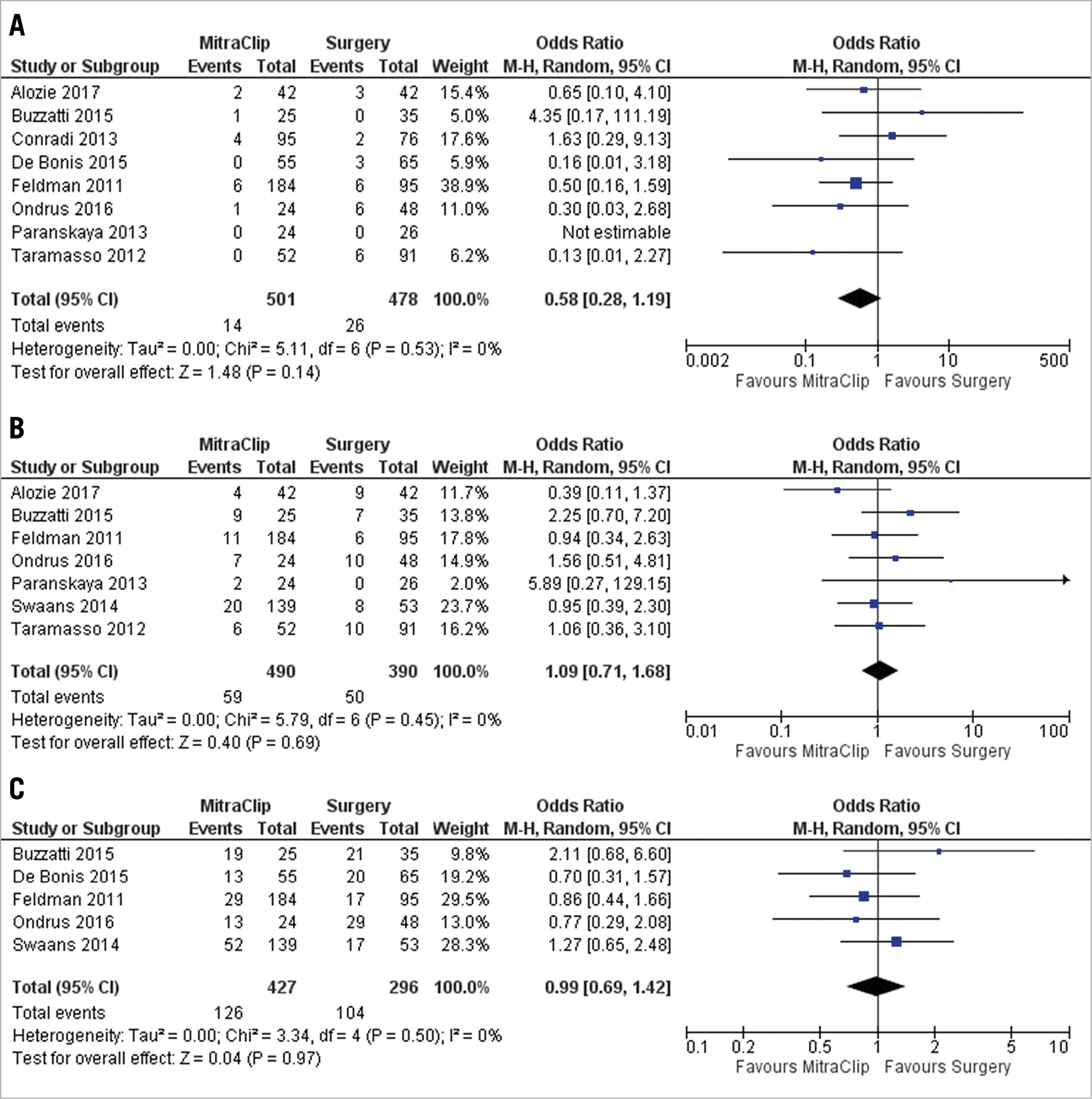
Figure 1. Forest plot of pooled odds ratios comparing MitraClip and MVS for mortality A) operative, B) 1 year and C) 3 years. M-H: Mantel-Haenszel method
Pooled in-hospital complications rates are listed in Table 3. MitraClip patients had higher early significant MR, 12% vs 1% (OR 4.6, 95% CI: 1.5-14, p=0.008) in eight studies; but lower bleeding rates 10% vs 27% (OR 0.26, 95% CI: 0.12-0.53, p<0.001) in five studies; and pacemaker implantation 0% vs 17% (OR 6.64, 95% CI: 3.78-11.6, p=0.01) in two studies compared to MVS patients, respectively.
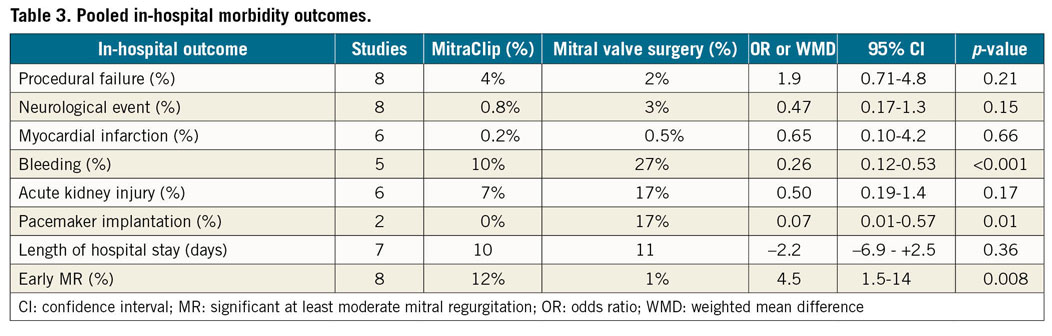
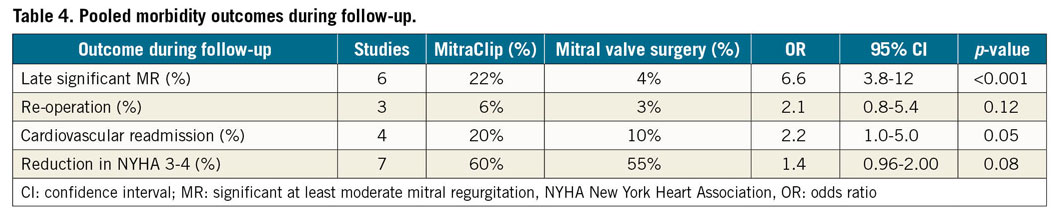
Table 4 shows a pooled analysis of long-term complication rates during follow-up. MitraClip patients had higher rates of late significant MR, 22% vs 4% (OR 0.15, 95% CI: 0.09-0.26, p<0.01) in six studies and cardiovascular readmission rates, 20% vs 10% (OR 2.2, 95% CI: 1.0-5.0, p=0.05) in four studies, with no differences in symptom improvement and re-operation.
Discussion
This meta-analysis compared the outcomes of the percutaneous MitraClip procedure with those of MVS for severe MR, with some important findings. In high-risk patients with primary or secondary MR, the MitraClip procedure had similar outcomes to MVS in terms of operative mortality, mortality at one year, and beyond. MitraClip patients had lower rates of periprocedural complications of bleeding and pacemaker implantation, whereas the rates of other complications such as stroke, myocardial infarction and acute kidney injury were similar to those of MVS. The disadvantages of the MitraClip procedure were higher rates of significant residual MR, both early and later on, as well as cardiovascular readmissions during follow-up.
Only one of the nine studies was a randomised trial (EVEREST-II)10,14, and the other eight observational studies contributed to the discrepancies in baseline characteristics between MitraClip and MVS candidates15,16,17,18,19,20,21,22. That MitraClip patients had higher baseline risk, with older age, a higher proportion of previous cardiac surgery, coronary artery disease and higher EuroSCOREs seen across the studies was not surprising as the MitraClip procedure was introduced as a potential alternative for patients who are either at high or prohibitive risk for MVS1,2. There is a wealth of experience for MVS as an effective strategy in low and intermediate risk MR candidates, with low operative mortality rates around 3% overall and good durability1,23. The corollary of this is that, had we found MitraClip patients had slightly worse outcomes than MVS, then it would be difficult to discern whether this was due to higher baseline risk or that the MitraClip procedure was truly inferior to MVS.
Despite the aforementioned differences at baseline, there were no differences in mortality outcomes between the two modalities. The pooled operative mortality rate of 3-5% is acceptable in this selectively higher risk cohort, and similar to that of all-comers undergoing either procedure for severe MR23. Operative mortality is an important safety measurement and long-term survival illustrates efficacy for valvular procedures. These results are especially reassuring for the MitraClip cohort, which had similar mortality rates to MVS, despite having higher baseline risk than MVS, and they highlight the utility of MitraClip in high-risk candidates warranting intervention, including those with ischaemic and functional MR and/or cardiomyopathy. Of note, the original EuroSCORE, which estimated operative mortality after cardiac surgery reported in these studies, grossly over-estimated that of MitraClip, estimated as 23% vs 3% actual, and to a lesser extent MVS, estimated as 11% versus 5% actual24. Although the more contemporary EuroSCORE II and STS scores were not routinely reported, they fit better with contemporary outcomes25,26,27. They can assist patient selection for the MitraClip procedure after determining which patients are at high risk for MVS. Unlike for MVS however, caution needs to be taken when applying these scores directly to the MitraClip procedure due to over-estimation and modest discriminative ability28.
Although procedural failure rates were relatively low, the main shortcomings of the MitraClip procedure are the high rates of residual MR, and possibly short- and long-term durability, being significantly worse than MVS. This finding was consistent across all studies10,13,14,15,16,17,18,19,20,21. Residual MR, especially moderate or severe, is to be avoided as it is associated with worse clinical outcomes19,30. Although this did not translate to statistically higher rates of reoperation during follow-up, this could have been because many of these high-risk at baseline candidates would have been ineligible or at too high a risk for reintervention. Whereas there are many MVS techniques to restrict residual MR, the MitraClip procedure, which mimics the Alfieri edge to edge surgical technique by clipping the two mitral valve leaflets together creating two small MV orifices, does not have the same capability9. Notably, most of the eligible studies in our meta-analysis used the earlier-generation MitraClip device and about half started enrolling patients before 2008, when the technique was in its infancy. With increasing experience over time, the reported early residual MR rate reduced to approximately 5% in the COAPT trial and contemporary registries13,31. Furthermore, a number of other percutaneous mitral valve intervention techniques are being developed and are in active clinical trials to try and overcome these shortcomings. These techniques include mitral annuloplasty, chordal replacement, mid-leaflet attachment to each side of small spacer (PASCAL system), ventricle remodelling and valve replacement32,33,34,35. Their reported rates of significant early MR are similarly at <5%.
Other periprocedural complications noted in the meta-analysis were either similar in occurrence (stroke, myocardial infarction and acute kidney injury) or higher for MVS (bleeding and pacemaker implantation). These findings are similar to other comparisons between transcatheter and surgical approaches to cardiovascular diseases, such as transcatheter versus surgical aortic valve replacement for aortic stenosis36,37. However, unlike transcatheter aortic valve implantation, the MitraClip procedure has a low risk of requiring pacemaker implantation as the MitraClip is deployed far from the heart’s native conduction system, whereas both mitral and aortic valve surgeries have significant risk of pacemaker implantation, typically at least 5%38. The proximity of the bioprosthetic aortic valve implanted by the transcatheter approach to the atrio-ventricular node increases the risk of heart block, requiring pacemakers at a rate comparable to those required following valve surgery36,37, whereas the landing zone for MitraClip is distant to the conduction system hence a low risk of pacemaker implantation (0% in our meta-analysis). Of some concern for the MitraClip procedure, however, is the higher rate of cardiovascular readmissions during follow-up compared to those for MVS in the pooled analysis, despite similar NYHA status. This is another important efficacy measure especially with many of these patients having heart failure admissions, likely in part due to greater residual MR and probably higher filling pressures for MitraClip. The hope is that with further experience and advances in percutaneous mitral valve techniques, cardiovascular readmissions may be reduced to similar rates as for MVS.
Secondary MR deserves a special mention, as the optimal interventional strategy remains controversial1,2. In our meta-analysis secondary MR was common at baseline in both arms, being present in 66-74% of patients, though there was a higher proportion of coronary artery disease in MitraClip vs MVS patients, with no differences in mortality endpoints. It is important to note that prior studies, including randomised trials, have not demonstrated a significant benefit for survival by performing MVS in addition to coronary artery surgery in the setting of secondary or ischaemic MR1,2,8,9. Two recent randomised trials specifically compared the MitraClip procedure with medical therapy for secondary MR with heart failure, with conflicting results12,13. The MITRA-FR trial found no difference between the MitraClip procedure or medical therapy alone in terms of death and heart failure hospitalisation12, whereas COAPT found significant reduction in both endpoints in favour of the MitraClip procedure13. The COAPT trial was larger, with longer follow-up, had higher heart failure biomarker levels and more severe MR that was disproportionate to the underlying cardiomyopathy’s remodelling of the left ventricle, as compared with the MITRA-FR trial, which may explain, in part, the discrepancy in their findings39. These sicker patients with secondary MR, both functional and ischaemic, are likely those to be targeted to benefit from MitraClip intervention.
Limitations
This meta-analysis has some limitations. The majority of studies were observational with inherent biases in patient selection and different baseline risk profiles which, as described earlier, influence the interpretation of the findings. There was also heterogeneity in study design including patient inclusion, aetiology of MR, intervention strategy, and type and timing of characteristics endpoints. Despite pooling nine studies, the overall sample size is moderate, at best, for determining differences in endpoints, especially ones which occur rarely or are infrequently reported. Comparison with a non-interventional medical approach was not assessed. Some important endpoints such as quality of life were not reported. Follow-up was also limited to, at most, five years. Longer-term durability and outcomes of the MitraClip procedure compared to MVS remain important unknowns, especially if the MitraClip procedure is being introduced to treat lower-risk and/or younger candidates in the future. Finally, the eligible studies took place between 2011-2017 and may not fully capture the contemporary experience, because the focus of more recent studies of the MitraClip procedure are either single-armed registries or comparisons with medical therapy for secondary MR or other percutaneous techniques, rather than MVS.
Conclusions
Patients with severe MR had similar mortality early and late after the MitraClip procedure compared to MVS, despite a higher baseline risk for MitraClip candidates. The main disadvantage of the MitraClip procedure is residual post-procedural MR in the short- and long-term and cardiovascular readmissions, whereas MVS had more periprocedural complications of bleeding and pacemaker implantation. A multidisciplinary and individualised approach with sound clinical judgement is required for deciding the optimal treatment modality for high-risk severe MR patients.
Impact on daily practiceThis meta-analysis of 9 studies and 1,171 patients showed that although percutaneous MitraClip patients have a higher baseline risk than MVS patients, mortality early, at one year and at three years were similar. MitraClip patients had higher rates of residual post-procedural MR and cardiovascular readmissions, but a lower risk of periprocedural complications, especially bleeding and pacemaker implantation, compared to MVS. MitraClip should be considered as an alternative to MVS particularly for high-risk candidates. |
Conflict of interest statement
The authors have no conflicts of interest to declare.

