When deciding between different treatment options for a patient with significant left main (LM) disease, stratification according to the risk of periprocedural and longer-term adverse clinical events is the cornerstone of the decision-making process. The presence of diffuse coronary artery disease, especially if accompanied by diabetes, favours surgical revascularisation, whereas percutaneous coronary intervention (PCI) is recommended in a growing number of patients with a SYNTAX score <331. If percutaneous treatment is decided, the anatomy of the distal LM bifurcation plays a defining role in choosing the appropriate stenting strategy. Crossover stenting of the main branch, in most cases the left anterior descending (LAD) artery, with additional treatment of the side branch (SB) only if needed, i.e., the provisional strategy, is the preferred approach for the majority of patients. A frequent dilemma pertains to the question of whether distal LM bifurcation lesions affecting both the LAD and circumflex (Cx) ostia would routinely require an upfront two-stent technique. So far, two randomised trials have addressed this question. The DKCRUSH-V trial (Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions) showed that routine SB stenting with the double kissing (DK) crush technique was superior to the provisional strategy in terms of the composite primary endpoint of 1-year target lesion failure (TLF) (5.0% vs 10.7%, respectively, hazard ratio [HR] 0.42, 95% confidence interval [CI]: 0.21-0.85; p=0.02)2. This difference was mainly due to the lower rates of target lesion revascularisation (TLR) and target vessel myocardial infarction (TVMI) in the DK crush arm. On the contrary, the EBC MAIN trial (The European Bifurcation Club Left Main Study) did not replicate these findings, showing no difference between provisional versus routine SB stenting in terms of its composite primary endpoint, including all-cause death, any MI and TLR at one year (14.7% in the provisional group vs 17.7% in the two-stent group; HR 0.8, 95% CI: 0.5-1.3; p=0.34)3. In the routine two-stent arm of the EBC MAIN trial, operators performed mainly culotte and T-/T and small protrusion (TAP) stenting (53% and 32%, respectively), with only 5% performing DK crush. Although, prima facie, the two trials show conflicting results, on closer inspection, there seems to be a common ground. Patients enrolled in the DKCRUSH-V trial seem to have had a more complex distal LM bifurcation anatomy with extensive Cx disease (median length 16 mm, as compared with 7 mm in the EBC MAIN trial). Previously, favourable results of the upfront two-stent technique for true bifurcations with an SB lesion length >10 mm had been confirmed in a network meta-analysis4. Moreover, a subanalysis of the DKCRUSH-V trial suggested that most of the benefit ascribed to the upfront SB stenting strategy was observed in the subpopulation of patients with Cx disease extending beyond 10 mm. Of note, in both trials the confidence intervals around the primary endpoint estimate were wide, suggesting a heterogeneity of the treatment effect in enrolled patients. This heterogeneity may have been, at least in part, the consequence of diverging effects of the provisional versus upfront two-stent technique in different anatomical subsets.
Therefore, the central question remains: how can we define a complex distal LM bifurcation anatomy that would require the upfront two-stent technique? The expert review by Chen et al in this issue of AsiaIntervention5 answers this question by advocating the use of the DEFINITION criteria that take into account the SB lesion length (>10 mm) and stenosis severity (>70%) as major criteria and the presence of multiple lesions, moderate/severe calcification and bifurcation angle <45% or >70% as minor criteria. If at least one major criterion plus any two minor criteria are present, then the upfront two-stent technique is advised. This argument is supported by the results of the DEFINITION-II trial (Two-stent vs Provisional Stenting Techniques for Patients With Complex Coronary Bifurcation Lesions), which showed that routine double stenting (78% DK crush) in patients with complex bifurcation lesions, according to the DEFINITION criteria, was associated with a lower TLF rate at 1 year (6.1% vs 11.4% in the provisional group, HR 0.52, 95% CI: 0.30-0.90; p=0.019), once again, mainly due to fewer TVMI and TLR6.
However, when interpreting the combined strong evidence from the DEFINITION-II trial and the DKCRUSH trial series, the following issues need to be carefully considered. First, in the DEFINITION-II trial, the rate of SB occlusion at any point during the procedure in the provisional arm was reported to be 8%, which may have contributed to the overall higher MI rate in patients undergoing provisional SB stenting. As highlighted in a recent European Bifurcation Club (EBC) consensus document, addressing procedural pitfalls of the provisional strategy may contribute to reducing periprocedural risks7. Second, historically, the DK crush technique has shown superiority over other two-stent techniques, such as culotte, primarily regarding the result at the SB ostium8. Recent focus on how to overcome the pitfalls of the culotte and T-/TAP techniques9, together with modifications such as double-kissing culotte, may contribute to a better result at the SB ostium. Third, despite favourable results reported up to 3 years in both the DKCRUSH-V and the DEFINITION-II trials, longer-term follow-up, beyond 5 and up to 10 years, has suggested increased mortality in patients treated with 2 stents10. Fourth, variables other than the choice of the stenting technique, such as operator experience11 and intracoronary imaging guidance12, have been shown to impact outcomes following LM PCI. Of note, in the DKCRUSH-V trial, enrolling operators were required to have had prior experience with DK crush stenting, whereas no such quality screening was performed for the provisional strategy. Moreover, imaging guidance was not standardised and was used in only ~40% of patients in both the DKCRUSH-V and EBC MAIN trials, rendering both intra- and inter-study comparisons difficult in terms of optimal immediate post-PCI result, regardless of the stenting technique.
In summary, in addition to anatomical landmarks on angiography recognised by the DEFINITION criteria, patient stratification according to the LM disease complexity may also need to incorporate intracoronary imaging, operator experience and an assessment of the risk of pitfalls for the chosen stenting technique (Figure 1), the ultimate goal being an objective definition of complex LM disease that may require 2 stents and avoiding the notion that complexity, like beauty, resides in the eye of the beholder.
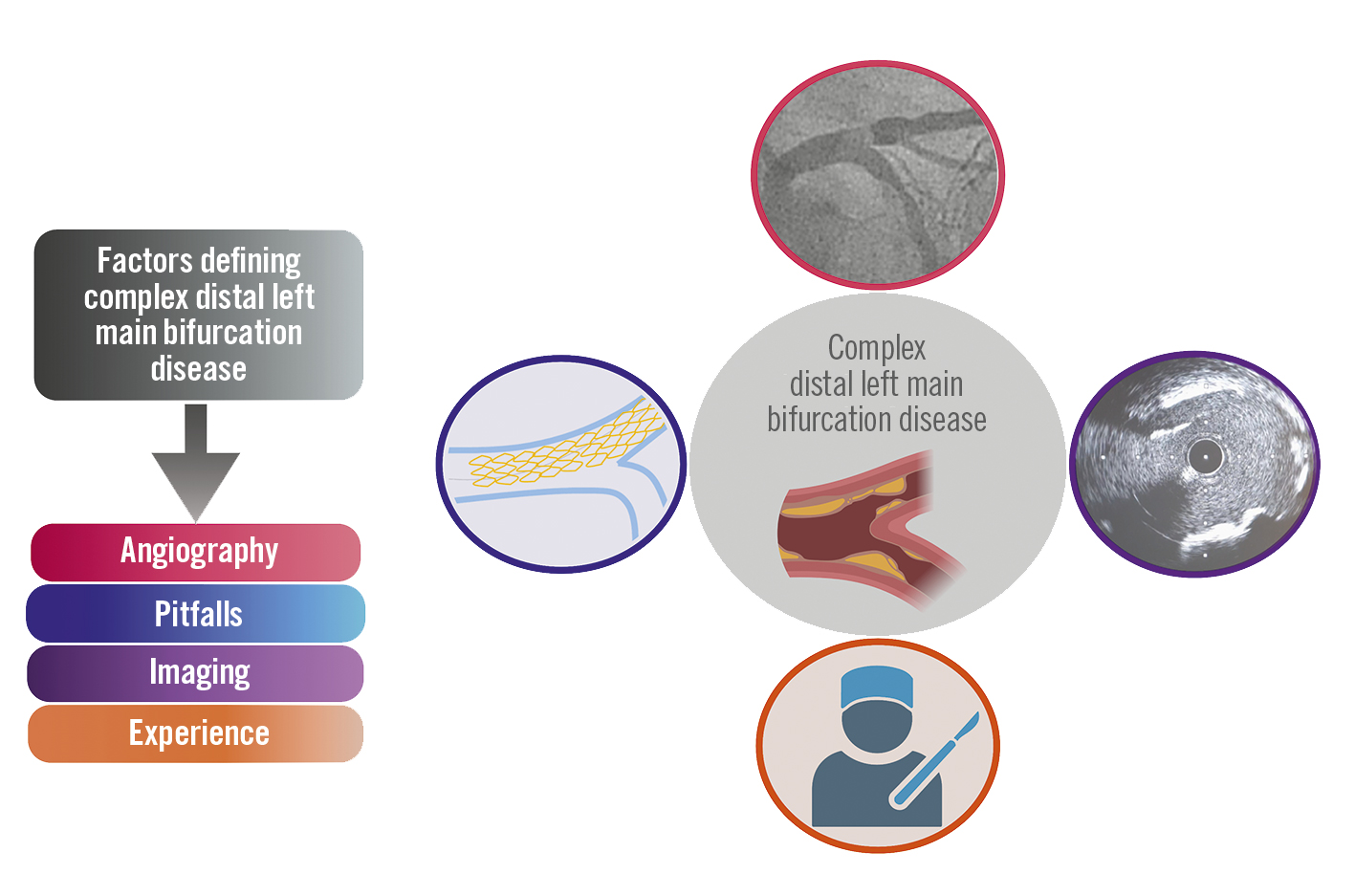
Figure 1. Multiple factors impacting outcomes of left main PCI beyond angiographic complexity. Created with BioRender.com. PCI: percutaneous coronary intervention
Conflict of interest statement
The author has no conflicts of interest to declare.
