An 81-year-old male presented with a history of diabetes, smoking, and chronic obstructive pulmonary disease (COPD). He was evaluated for angina on exertion, which was stratified using a nuclear medicine study and revealed severe ischaemia in three territories. The diagnostic angiography revealed a severe left anterior descending artery (LAD) lesion, a right coronary artery (RCA) with diffuse disease (angiographically, mild calcification was observed), and an anomalous origin of the left circumflex artery (LCx) in the right coronary sinus (Figure 1A, Moving image 1) with an intermediate lesion in the distal segment. Percutaneous coronary intervention (PCI) was performed in the first segments of the LAD and the LCx without any complications.
Subsequently, an RCA intervention was performed. A Judkins right (JR) 3.5, 6 Fr catheter was chosen, and using the buddy wire technique (Figure 1B), the guide was advanced to the distal segment of the RCA (Figure 1C). We attempted to predilatate with a 2.0×12 mm balloon, but we were unable to cross the lesion (Figure 1D). We opted to use a GUIDEZILLA catheter (Boston Scientific) and the smallest possible balloon to try to pass the lesion (1.0×15 mm), but we were unable to achieve the objective (Figure 1E). We attempted to advance a Finecross microcatheter (Terumo), but we were unsuccessful due to a lack of support (Figure 1F).
Given the difficulty in crossing the lesion with the balloon and the absence of a rotational atherectomy device, we decided to advance a Runthrough NS Hypercoat (Terumo) guide to the posterolateral branch of the LCx to stabilise the JR catheter (Figure 1G). We performed active anchoring in the posterolateral branch of the circumflex with a 2.0×15 mm balloon at the level of the previously placed stent, and simultaneously, we advanced the 1.0×15 mm balloon to the RCA, managing to cross the site of maximum narrowness (Figure 1H, Moving image 2). Sequential predilatation was performed from distal to proximal with the following Ryurei balloons (Terumo): 1.0×5 mm, 1.25×15 mm, 2.0×15 mm, and 2.5×15 mm (Figure 1I, Moving image 3). Subsequently, we advanced a GUIDEZILLA catheter to the distal segment of the RCA to assist the advancement of the stent and removed the guidewire and the circumflex artery balloon. Guided by intravascular imaging, we placed a 2.5×38 mm durable-polymer (DP) stent in the distal RCA, a 3.0×48 mm stent in the distal to the mid-segment, and a 4.0×38 mm stent in the mid-ostial proximal segment. In the angiographic control, Thrombolysis in Myocardial Infarction grade 3 distal flow was observed (Figure 1J, Figure 1K, Moving image 4), without any complications.
Failure to cross severely calcified lesions with a balloon after successful guidewire crossing is a common cause of PCI failure12. Although only mild calcification of the RCA was observed in this patient’s diagnostic angiography, during the procedure we were faced with an uncrossable lesion.
In cases with balloon-uncrossable coronary lesions, the percutaneous coronary rotational atherectomy is an appropriate strategy as an injury-modifying therapy which can greatly facilitate lesion crossing with a balloon. However, it requires wire exchange for a dedicated 0.009” ROTAWIRE (Boston Scientific), which may not be feasible in cases with high calcification34. In our case, this strategy was one of two options for treating the injury; however, at the time of the procedure, we did not have the device available to us, so we opted for the alternative strategy with an anchoring balloon in the circumflex artery.
The balloon anchoring strategy is an appropriate technique to provide greater support for the guide catheter during complex PCI procedures. Normally, balloon anchoring is done in a side branch (usually a conus or acute marginal branch for the RCA, or a diagonal or obtuse marginal for LCx or the LAD)34. However, it should be noted that care should be taken not to damage the side branch (coronary dissection). In our case, having an emerging vessel in the same sinus and with the presence of a stent in the posterolateral branch, we decided to anchor the balloon in the LCx instead of in the conus artery.
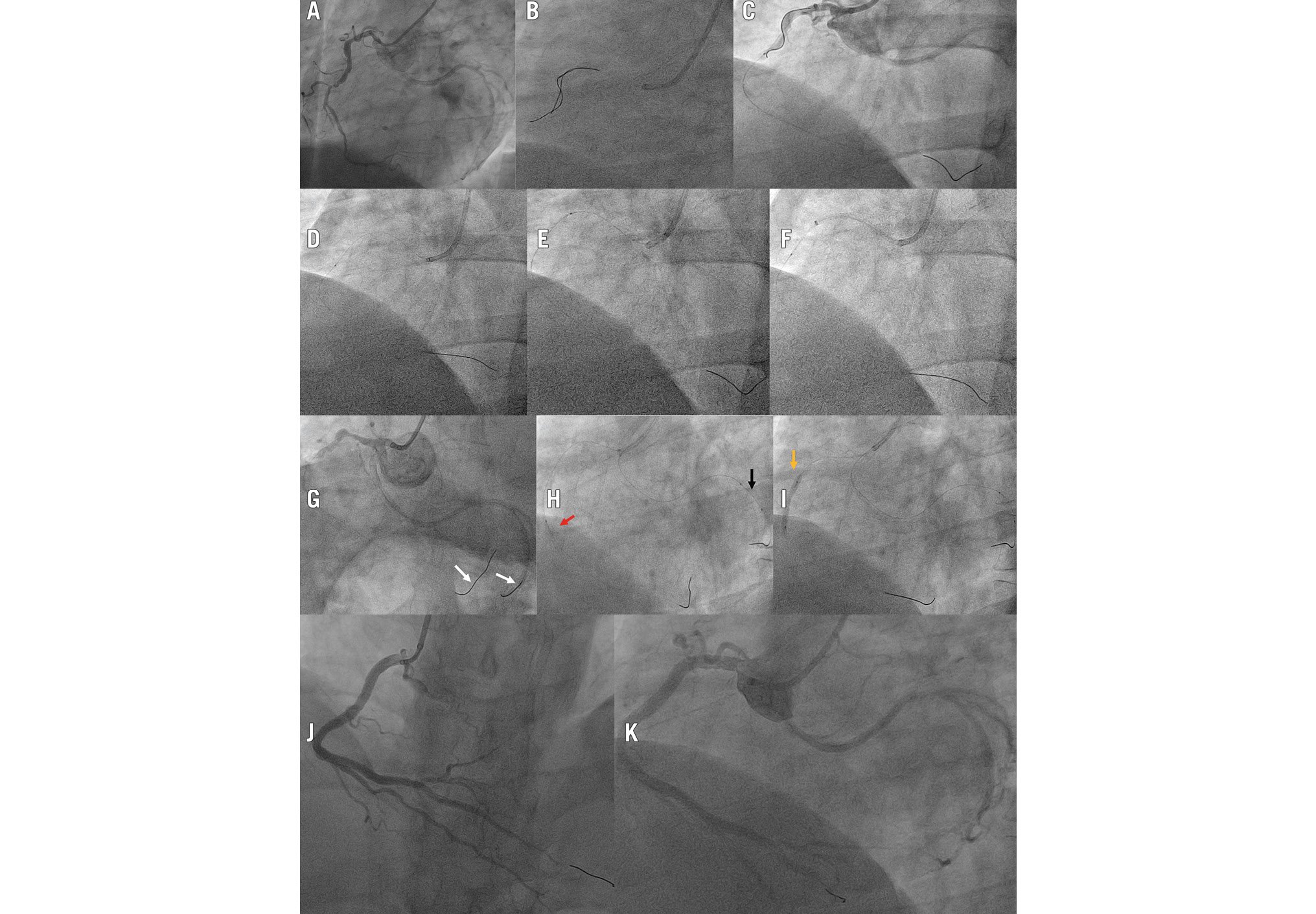
Figure 1. The procedure, step-by-step. A) Diagnostic angiography. RCA with diffuse lesion and circumflex artery originating from the right coronary sinus. B) and (C) Buddy wire technique to overcome the lesion. D) through (F) shows the unsuccessful attempts to cross the lesion. D) Use of a 2.0×15 mm balloon to try to cross the injury in a conventional way. E) Use of a 1.0×15 mm balloon supported by a catheter extender. F) Microcatheter and catheter extender. G) through (I) demonstrates the anchoring balloon technique in the circumflex artery. G) Guidewire in the RCA and circumflex artery (white arrows, dummy wire technique). H) Inflation of the anchoring balloon in the circumflex artery (black arrow) and simultaneous advancement of the 1.0×15 mm balloon to cross the RCA lesion (red arrow). I) Predilatation of the right coronary lesion (yellow arrow). J) The procedure resulted in TIMI grade 3 RCA flow. K) Indirect angiographic control to visualise both arteries. RCA: right coronary artery; TIMI: Thrombolysis in Myocardial Infarction
Conflict of interest statement
The authors have no conflicts of interest to declare.
