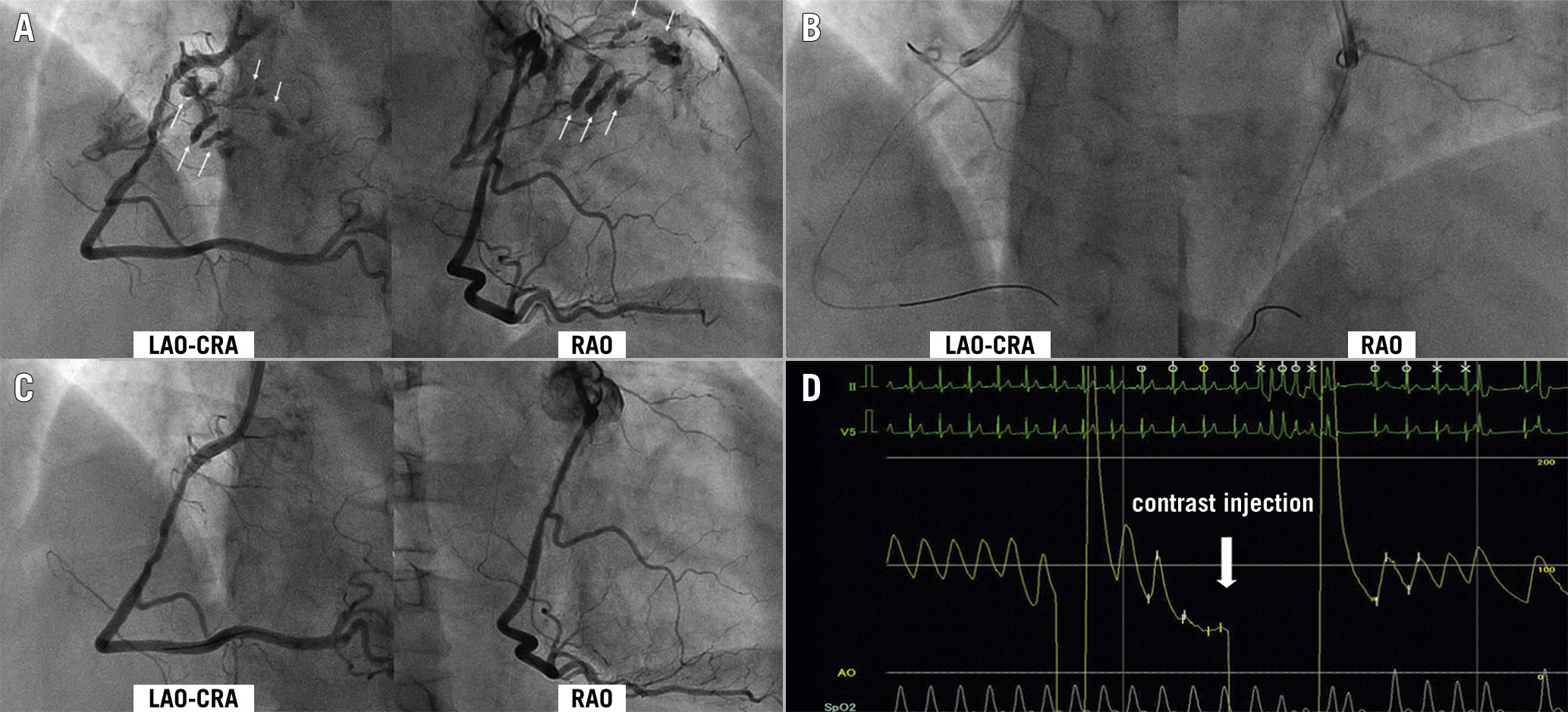
Figure 1. Coronary angiography and pressure waveform. A) Coronary angiography revealed multiple coronary perforations (arrows) (Moving image 1 and Moving image 2). B and C) Contrast injection from the microcatheter and final angiography revealed the coronary perforations were haemostatic (Moving image 3-Moving image 6). D) Pressure waveform at the tip of the diagnostic catheter showed wedged pressure just before contrast injection. LAO-CRA: left anterior oblique cranial view; RAO: right anterior oblique view
A 54-year-old woman with a history of dyslipidaemia presented with effort angina. Coronary angiography (CAG) was performed to investigate effort angina. A 4 Fr Judkins right (JR) 4.0 diagnostic catheter was inserted into the right coronary artery (RCA). After 6 ml of contrast medium was injected at 2.5 ml/s using a mechanical automated injector with a pressure limit of 300 psi, multiple coronary perforations were observed from the periphery of the conus branch (Figure 1A, Moving image 1, Moving image 2). A 7 Fr JR 4.0 guiding catheter was inserted into the RCA. Contrast injection from the microcatheter placed in the conus branch showed that the coronary perforations had already achieved haemostasis spontaneously (Figure 1B, Moving image 3, Moving image 4). On rechecking 10 minutes later, the coronary perforations were completely haemostatic (Figure 1C, Moving image 5, Moving image 6). The patient remained haemodynamically stable, and bedside echocardiography revealed no pericardial effusion. Retrospectively, the pressure waveform at the tip of the diagnostic catheter showed wedged pressure just before contrast injection (Figure 1D). The possible mechanism of the multiple coronary perforations in this case could be that the diagnostic catheter was wedged in the conus branch and contrast was injected, which increased the pressure in the conus branch and caused the distal conus branch to rupture.
Coronary perforation is a serious complication, usually caused by a wire or balloon during percutaneous coronary intervention. To the best of our knowledge, this is the first report of coronary perforations due to CAG alone. Contrast injection with a wedged catheter can result in an iatrogenic catheter-induced ostial coronary artery dissection, but in this case, it caused coronary perforations. Although obvious, it is important to pay attention to the pressure waveform just before contrast injection. In cases where the catheter is easily inserted into the conus branch, manual contrast injection by hand while feeling resistance may be safer. It must be taken into account that even a mere diagnostic CAG can lead to the complication of coronary perforation.
Conflict of interest statement
The authors have no conflicts of interest to disclose.
