Introduction
Over the past few decades, clinical trials have indicated that patients with diabetes and coronary artery disease (CAD) have suboptimal outcomes after revascularisation when compared with patients without diabetes1. Patients with diabetes typically exhibit disruptions in metabolic processes that can potentially contribute to increased platelet reactivity, leading to early development of atherosclerosis, cardiomyocyte dysfunction, and renal failure through various mechanisms23. Further, vascular endothelial dysfunction and enhanced smooth muscle proliferation accelerate the response to injury and trigger higher event rates following percutaneous coronary intervention (PCI)4. Multivessel involvement and diffuse disease associated with diabetes make the scenario even tougher, resulting in worse clinical outcomes5. The optimal treatment strategy for patients with diabetes and multivessel disease (MVD) has long been a concerning issue to physicians.
The Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease (FREEDOM) trial was a landmark trial conducted between 2005 and 2010 to compare coronary artery bypass grafting (CABG) with PCI. The study population included 1,900 patients with diabetes and angiographically confirmed multivessel CAD, with stenosis of more than 70% in two or more major epicardial vessels involving at least two separate coronary artery territories. Of the enrolled patients, 82% and 85% had triple vessel disease in the PCI group and in the CABG group, respectively, and 91% of patients had left anterior descending artery (LAD) involvement. The trial excluded patients with significant left main stenosis. It aimed to determine the optimal revascularisation strategy for this specific patient population on aggressive medical therapy. First-generation sirolimus-eluting and paclitaxel-eluting stents were used in 51% and 43%, respectively, of patients who actually underwent PCI. The use of abciximab was recommended for patients undergoing PCI. The use of dual antiplatelet therapy (DAPT) with aspirin and clopidogrel was recommended for at least 12 months after stent implantation. The primary outcome was a composite of death from any cause, non-fatal myocardial infarction (MI), and non-fatal stroke6.
The results of the FREEDOM trial, with a median follow-up of 3.8 years6, were published in 2012 and demonstrated that, at 30 days, the primary outcome occurred in fewer patients in the PCI group than in the CABG group (2.7% vs 4.4%). The rate of cardiovascular death (63.7% of all deaths) did not differ significantly between the two study groups (p=0.12 by the log-rank test), nor did the rate of major adverse cardiovascular and cerebrovascular events (MACCE) at 30 days (p=0.68 by the log-rank test). However, at 1 year after the procedure, there was a significant difference in the rate of MACCE, with 16.8% in the PCI group versus 11.8% in the CABG group (p=0.004), a difference attributed largely to the occurrence of repeat revascularisation events up to 1 year in the PCI group. Furthermore, the 5-year event rate was 26.6% in the PCI group, compared with 18.7% in the CABG group. In the FREEDOM follow-on study, the all-cause death rate up to 8 years continued to be significantly higher (24.3% vs 18.3%) with PCI (hazard ratio [HR] 1.36, 95% confidence interval [CI]: 1.07-1.74)7. There were fewer strokes in the PCI group than in the CABG group (22 vs 37; p=0.03) during the follow-up of more than 5 years. The excess of strokes in the CABG group occurred in the first 30 days after randomisation (0.3% vs 1.8%; p=0.002). Specifically, CABG reduced the risk of MACCE, such as MI and death, when compared to PCI. This study suggested that CABG should be the preferred revascularisation strategy for patients with diabetes and MVD. Similar results have been reported for patients with type 1 diabetes specifically8.
Since the publication of the FREEDOM trial, there has been much discussion and research around the question of the optimal management of CAD in diabetic patients. In a meta-analysis that included a total of 27 studies (2006-2021), Jaiswal et al compared the long-term cardiovascular outcomes of PCI versus CABG among patients with diabetes and MVD. Compared with the CABG group, the PCI group had higher odds of overall all-cause mortality (odds ratio [OR] 1.18, 95% CI: 1.02-1.37; p=0.03), MACCE (OR 1.52, 95% CI: 1.31-1.75; p=0.00), MI (OR 1.85, 95% CI: 1.46-2.36; p=0.00), repeat revascularisation (OR 3.08, 95% CI: 2.34-4.05; p=0.00) and cardiac death (OR 1.27, 95% CI: 1.02-1.59; p=0.04), while the odds of cerebrovascular accident (CVA; OR 0.57, 95% CI: 0.37-0.86; p=0.01) was higher in the CABG group. The meta-analysis concluded that patients with diabetes and multivessel CAD had better cardiac outcomes after CABG as compared to PCI. However, the incidence of CVA was significantly higher after CABG9. In another analysis, by Head et al, CABG had a mortality benefit over PCI in patients with MVD, particularly those with diabetes and higher coronary complexity. However, no benefit for CABG over PCI was seen in patients with left main disease10. In a patient-level pooled analysis that included around 5,034 patients from 3 federally funded trials, at a median of 4.5 years of follow-up, CABG+optimal medical therapy (OMT) was superior to PCI+OMT for the primary endpoint (HR 0.71, 95% CI: 0.59-0.85; p=0.0002), death (HR 0.76, 95% CI: 0.60-0.96; p=0.024), and MI (HR 0.50, 95% CI: 0.38-0.67; p=0.0001), but not stroke (HR 1.54, 95% CI: 0.96-2.48; p=0.074)11. Nevertheless, a major limitation of the available comparative literature is that only a limited number of studies used new-generation drug-eluting stents (DES); hence, the outcomes of PCI with these newer DES were not compared with CABG in diabetic patients. Moreover, medical therapy has significantly advanced since the time of FREEDOM, with more potent antiplatelet therapy (prasugrel, ticagrelor), better antidiabetic therapy (sodium-glucose cotransporter-2 [SGLT2], glucagon-like peptide-1 [GLP-1] antagonists vs insulin and thiazolidinedione) and more potent lipid-lowering therapy (proprotein convertase subtilisin/kexin type 9 [PCSK9] inhibitors). Another limitation is that there was no comparison between both types of revascularisation modality and medical treatment among these various studies. Further, more than 95% of patients enrolled in most trials like the FREEDOM trial had preserved left ventricular ejection fraction. Outcomes of revascularisation strategies may differ in patients with diabetes, left main disease and low systolic left ventricular function. Additionally, it must be noted that survival, MI and repeat revascularisation are not the sole critical outcomes of interest to physicians and patients; alleviating ischaemic symptoms, thus improving quality of life, also stands out as an important objective. Though the findings of the FREEDOM trial greatly impacted the way clinicians approached revascularisation in diabetic patients with MVD, much has changed both in PCI technology and in the management of diabetes since the publication of the FREEDOM trial (Figure 1). The aim of this review is to re-evaluate the results and applicability of the FREEDOM trial in patients with diabetes and MVD, as per current advancements in technology.
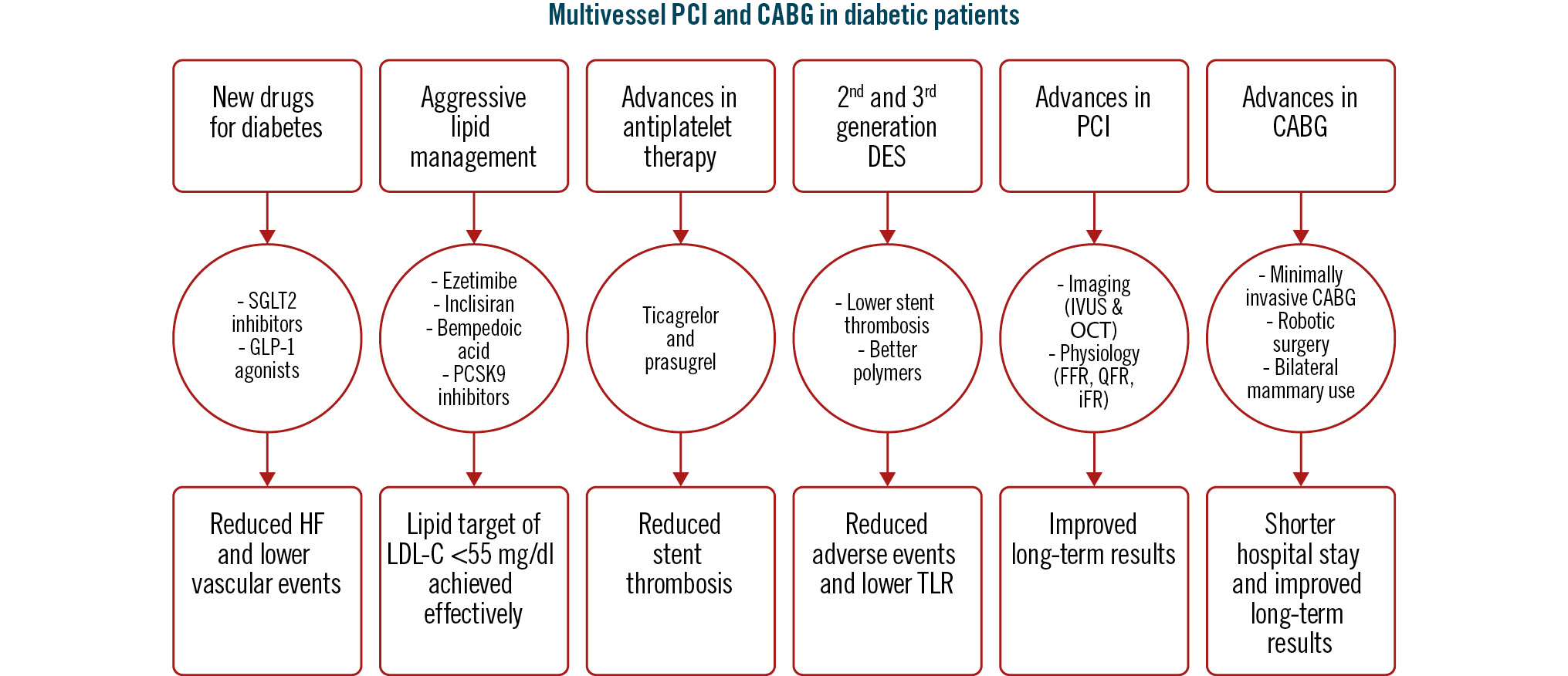
Figure 1. Improvements following the FREEDOM trial. CABG: coronary artery bypass grafting; DES: drug-eluting stent; FFR: fractional flow reserve; GLP-1: glucagon-like peptide-1; HF: heart failure; iFR: instantaneous wave-free ratio; IVUS: intravascular ultrasound; LDL-C: low-density lipoprotein cholesterol; OCT: optical coherence tomography; PCI: percutaneous coronary intervention; PCSK9: proprotein convertase subtilisin/kexin type 9; QFR: quantitative flow ratio; SGLT2: sodium-glucose cotransporter-2; TLR: target lesion revascularisation
Improved percutaneous coronary intervention technologies and results
New PCI technologies that could have an impact on patients with diabetes involve more compatible stent platforms, improved biocompatibility of polymer coatings on stents, low and ultra-low thickness of stent struts, re-engineered bioresorbable vascular scaffolds, and better and safer drugs coated over the stents. Earlier generations of stents used paclitaxel as the antiproliferative drug; with the evolution of technology, the use of everolimus and sirolimus have shown improved outcomes. TUXEDO-India has already shown the superiority of everolimus over paclitaxel, the drug used in one of the stents in the FREEDOM trial12. Newer devices for debulking, including intravascular lithotripsy13, and the use of intravascular imaging in patients with diabetes1415 have also widened the use of PCI to lesions which were previously reserved for CABG.
Advances in this area could reduce inflammation and thrombogenicity, and allow improved vessel healing and rapid endothelial coverage, with the added advantage of preventing restenosis, as well as mitigating some of the adverse vascular effects of diabetes1617. In this context, the ongoing TUXEDO-2 India trial has been designed to primarily compare the clinical outcomes of PCI with the new-generation ultrathin-strut Supraflex Cruz (Sahajanand Medical Technologies Ltd.), compared to the widely used second-generation stent, XIENCE (Abbott), in the setting of contemporary optimal medical and antiplatelet (prasugrel/ticagrelor) therapy in Indian patients with diabetes and MVD (85% triple vessel disease). The secondary objective of the TUXEDO-2 India study is to assess clinical outcomes by comparing a combined group from both study arms (Supraflex Cruz+XIENCE; PCI arm) versus CABG, based on a performance goal derived from the CABG arm of the FREEDOM trial (historical cohort). As a tertiary objective, a further randomisation will evaluate the comparative efficacy and safety of ticagrelor versus prasugrel among patients with diabetes and MVD. Figure 2 demonstrates the study design of TUXEDO-2 India study. The details of the study design are published elsewhere18. Enrolment for the trial started in February 2020 at 70 clinical sites in India. A total of 1,561 patients have been enrolled as of 26 March 2024; the results of the trial are anticipated in late 2025. This ongoing trial, featuring new-generation DES and contemporary medical treatment, will help to investigate whether the outcomes observed in the FREEDOM trial would have been altered in the present era.
Further, the use of intravascular imaging and physiology-guided PCI can improve outcomes after PCI in the current scenario, when compared to the outcomes of PCI with the earlier-generation stents used in the FREEDOM trial19. Conducting a systematic physiological evaluation of coronary lesions in patients with diabetes, which includes assessing their “functional SYNTAX score” instead of relying solely on anatomical criteria, enables the reclassification of diabetic patients with MVD into a lower SYNTAX category (≤32). This reclassification paves the way for the application of optimised PCI strategies in these individuals. Non-invasive functional assessment of coronary lesions can be helpful to guide coronary interventions and identify patients with diabetes who would derive similar benefits with PCI compared to CABG20. In line with this perspective, the FIRE trial, published in 2023, focused on older patients (≥75 years) with MI and multivessel disease undergoing PCI with the newer-generation DES, Supraflex Cruz. It assigned patients to receive either physiology-guided complete revascularisation of non-culprit lesions using various assessment methods or no further revascularisation beyond the culprit lesion. The trial reported that those who underwent physiology-guided complete revascularisation had a reduced risk of a composite of death, MI, stroke, or ischaemia-driven revascularisation at 1 year compared to those who received culprit-lesion revascularisation only21. Further, in a systematic review, Faro et al emphasised optimal timing and the use of various guidance strategies (complexity, intracoronary imaging, non-invasive imaging, physiology, renal function, inflammation, haemodynamic support) for complete revascularisation in patients with MVD and suggested personalised approaches with a comprehensive evaluation by a Heart Team22.
The literature623 as well as the latest 2023 American Heart Association (AHA)/American College of Cardiology (ACC) guidelines on chronic coronary disease (CCD) recommend that PCI may be considered as an alternative to CABG to reduce the incidence of major adverse cardiovascular events in patients with CCD and diabetes who have left main stenosis and low- or intermediate-complexity CAD (e.g., SYNTAX score ≤33)24. Further, the 2023 European Society of Cardiology (ESC) guidelines for patients with diabetes state that complete revascularisation is recommended in patients with ST-segment elevation myocardial infarction (STEMI) and non-ST-elevation acute coronary syndrome without cardiogenic shock and with multivessel CAD25. Moreover, the 2021 ACC/AHA/Society for Cardiovascular Angiography & Interventions (SCAI) guideline for coronary artery revascularisation suggested that in patients with diabetes and multivessel CAD with the involvement of the LAD, who are appropriate surgical candidates, CABG (with a left internal mammary artery to the LAD) is recommended in preference to PCI to reduce mortality and repeat revascularisations. On the other hand, the guidelines recommended that in patients with diabetes who have multivessel CAD amenable to PCI and an indication for revascularisation and who are poor candidates for surgery, PCI can be useful to reduce long-term ischaemic outcomes26. In a study based upon propensity-based matching from the New York State registry evaluating the results of PCI or CABG in diabetic patients with MVD, Bangalore et al27 showed that PCI using everolimus-eluting stents was associated with lower rates of death and stroke in the short term and with similar mortality and lower stroke rates but higher MI rates in the longer term when compared with CABG. However, the MI rates were higher only in patients with incomplete revascularisation after PCI. These observations bring the results of PCI using current-generation DES closer to those of CABG in a similar patient population to that studied in the FREEDOM study.
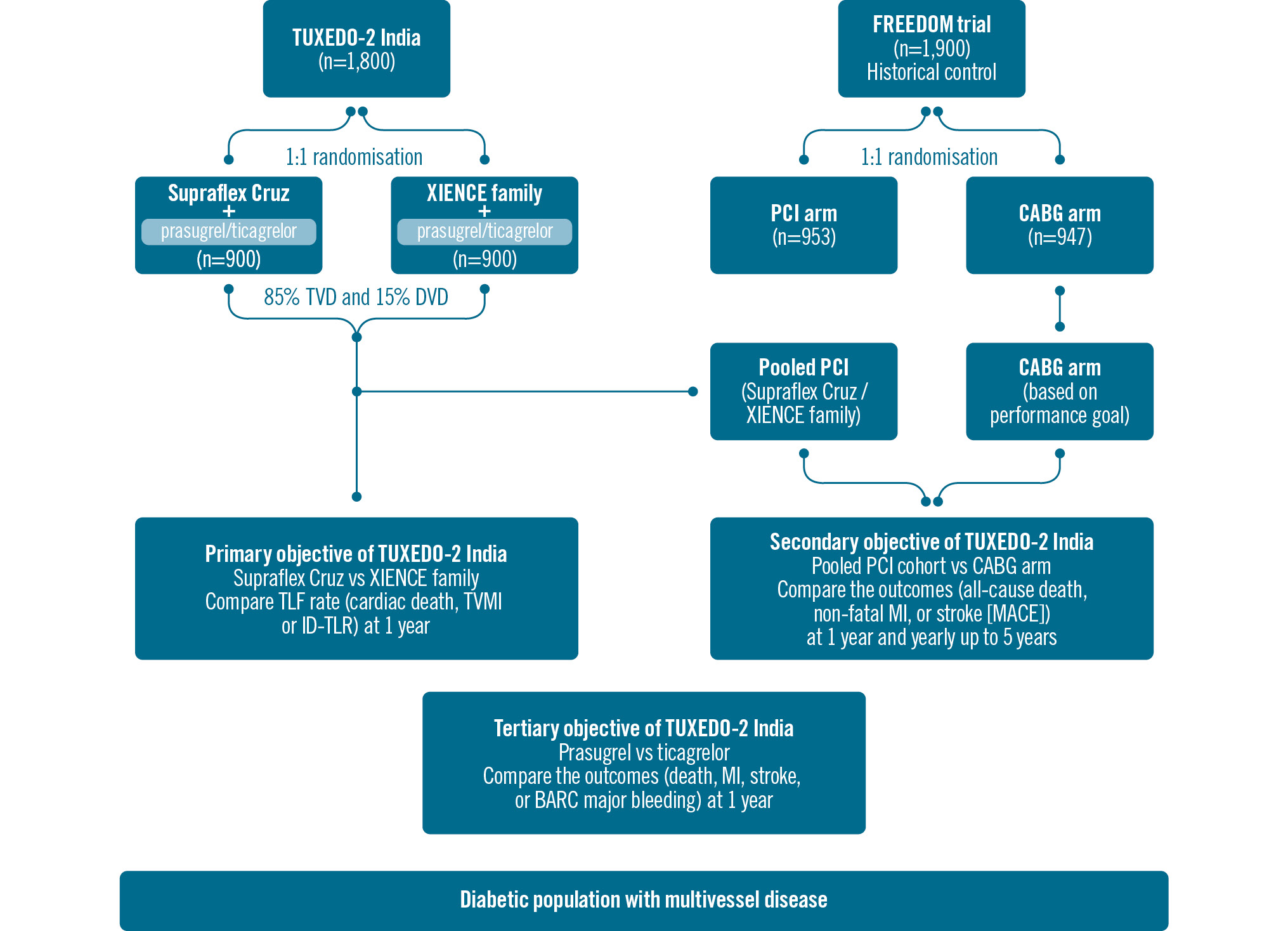
Figure 2. Line diagram of TUXEDO-2 India study protocol. BARC: Bleeding Academic Research Consortium; CABG: coronary artery bypass grafting; DVD: double vessel disease; ID-TLR: ischaemia-driven target lesion revascularisation; MACE: major adverse cardiovascular events; MI: myocardial infarction; PCI: percutaneous coronary intervention; TLF: target lesion failure; TVD: triple vessel disease; TVMI: target vessel myocardial infarction
Refinements in dual antiplatelet therapy
The main aim of utilising DAPT differs in patients undergoing PCI and in those undergoing CABG. In CABG patients, the primary goal is the prevention of atherothrombotic events, whereas in PCI patients, the focus is on reducing the risk of stent thrombosis. Regarding the use of DAPT in patients with diabetes, several studies have independently investigated its duration and associated outcomes in both CABG and PCI patients. A post hoc, non-randomised analysis based on data from the FREEDOM trial, which focused on patients who had undergone CABG, was conducted by van Diepen et al. Their findings revealed that a greater number of patients with diabetes were prescribed DAPT as compared to aspirin monotherapy. Furthermore, when comparing the DAPT group to those receiving aspirin monotherapy, there were no associated differences in terms of cardiovascular or bleeding outcomes28. In another study, conducted by Yamamoto et al, the safety and efficacy of clopidogrel monotherapy were evaluated after very short DAPT in patients with diabetes undergoing PCI. The study concluded that, compared to a 12-month DAPT regimen, clopidogrel monotherapy following only 1 month of DAPT reduced the occurrence of major bleeding events without an increase in cardiovascular events29. Ticagrelor and prasugrel have been shown to be more effective antiplatelet drugs in patients with ACS3031. In a recent study comparing ticagrelor versus prasugrel in patients with ACS, prasugrel was found to be superior regarding the composite of death, MI and stroke at 1 year32. Such a comparison has not been made in an exclusively high-risk, diabetic population; this is one of the objectives of the TUXEDO-2 India study. Results of other ongoing trials such as OPTIMUS-7 (ClinicalTrials.gov: NCT04484259) and TIGER-diabetes (ClinicalTrials.gov: NCT04307511) are also awaited. Thus, the optimal DAPT regimen in a complex diabetic patient population with multivessel disease undergoing PCI remains to be determined.
Irrespective of the chosen revascularisation approach, patients with diabetes continue to face a heightened risk of recurrent cardiovascular events. It is imperative to widely implement multidisciplinary disease management programmes designed to enhance treatment outcomes in patients with diabetes. These programmes should encompass various therapeutic objectives, such as the utilisation of potent antiplatelet medications, stricter glycaemic control with novel antidiabetic drugs, and intensive lipid-lowering strategies.
Improved outcomes with newer glycaemia-controlling drugs and adjuncts
In the context of pharmacological therapies, there is a strong suggestion for broadening the utilisation of SGLT2 inhibitors in patients with diabetes who have confirmed atherosclerotic disease20. This recommendation is rooted in clinical trial data demonstrating a reduced risk of cardiovascular events associated with SGLT2 inhibitors33. Likewise, studies have suggested that alpha-glucosidase inhibitors, which inhibit carbohydrate absorption from the small intestine, could decrease the risk of cardiovascular disease in patients with diabetes34. Moreover, GLP-1 agonists represent a promising advancement in diabetes pharmacotherapy35, as they stimulate insulin secretion in a glucose-dependent manner, slow down gastric emptying to suppress appetite, and have demonstrated a decrease in cardiovascular events in some recent trials363738. In combination with new and improved drugs, continuous glucose monitoring can lead to better control of blood sugar, ultimately leading to better overall health outcomes in patients with diabetes. Recent findings have indicated a link between high glucose variability and the progression of vascular complications in patients with diabetes. Continuous glucose monitoring has shown associations with factors such as carotid intima-media thickness, heightened arterial stiffness, as well as increased risks of all-cause mortality and cardiovascular mortality39.
Stricter targets of low-density lipoprotein cholesterol lowering to <55 mg/dl in high-risk patients have improved the outcomes in diabetic patients with CAD. The availability of non-statin agents, like ezetimibe, bempedoic acid and PCSK9 inhibitors, has made this target possible for most patients in present times40.
Need for the reappraisal of optimal revascularisation therapy in diabetic patients with multivessel disease
While clinical trials like the FREEDOM trial offer the most robust evidence regarding the comparative effectiveness of different therapies, they represent the average outcomes of treatments among randomised patient groups. Since every patient is unique, and there is no such thing as a truly “average” patient, applying these findings to individual patients in everyday clinical practice can be challenging41. The literature also recommends that the choice between CABG and PCI for patients with diabetes and MVD should be made on a case-by-case basis, bearing in mind the patient’s clinical profile and preferences. Factors such as vessel anatomy, diabetes control, age, and other comorbidities should also be taken into account. Recent literature suggests that patients with diabetes and MVD presenting with STEMI and a suitable anatomy should undergo PCI of the culprit lesion as the first-line revascularisation option2526. This should be followed by a Heart Team consultation to discuss whether medical therapy, PCI or CABG would be more suitable for the remaining significant obstructive CAD. Further, the recent 2021 ACC/AHA/SCAI guideline for coronary artery revascularisation recommends that, in patients for whom the optimal treatment strategy is unclear, a Heart Team approach which includes representatives from interventional cardiology, cardiac surgery, and clinical cardiology is recommended to improve patient outcomes. Ideal situations for Heart Team consideration include patients with complex coronary disease, those with comorbid conditions that could impact the success of the revascularisation strategy, and other clinical or social situations that may impact outcomes26.
Although the predominant evidence from trials favours CABG in patients with diabetes and multivessel disease, PCI remains a common revascularisation strategy in the real world despite guidelines recommending CABG based upon the FREEDOM trial results. However, a general feeling amongst cardiologists is that patients with heightened surgical risk due to individualised factors should undergo PCI, when a less invasive procedure may be the favourable choice. The existence of institutional variation or institutional culture is also an important determinant of the favourability towards PCI42. Accordingly, Qintar et al prepared models that can help disseminate the best treatment recommendations by showing both physicians and patients the expected benefits and risks of CABG compared with multivessel PCI. Clinicians can use an online risk prediction tool calculator, and personalised estimates based on the models can be calculated41. The tool aims to facilitate informed discussions by transparently presenting the risks and benefits of both procedures. By addressing barriers in clinical care, such as patient preference and perceived risks, these tools could promote evidence-based, patient-centric care. However, we recommend further investigation into the use of these risk models in routine clinical care to gauge their impact on the adoption of clinical trial results and patient outcomes.
Quality of life and outcomes with revascularisation
During the initial days after revascularisation, PCI has shown more rapid improvement in health status and quality of life compared with CABG. Gradually, as time has passed, no consistent, significant differences remain in health status or quality-of-life domains between the CABG and PCI strategies43. In an analysis of quality of life in patients enrolled in the FREEDOM trial, Abdallah et al found that over 70% of patients experienced freedom from angina with both PCI and CABG at each follow-up interval. Differences between treatment groups regarding various aspects of cardiovascular wellbeing − such as physical constraints, overall quality of life, and breathlessness − were consistently marginal43. Additionally, the results from the EXCEL Trial related to quality of life also showed that quality of life is better with PCI than with CABG, in terms of faster relief of angina (better Seattle Angina Questionnaire score), better physical activity, and higher treatment satisfaction44. While technologies for CABG have advanced and have become less invasive − with developments such as arterial grafting using the radial artery and bilateral internal thoracic artery, no-touch saphenous vein grafting, minimally invasive surgical CABG, robot-assisted CABG, and total endoscopic CABG − the prolonged recovery period associated with CABG remains a concern. Consequently, PCI has emerged as a viable alternative for patients with limited life expectancy (attributed to factors such as advanced age or multiple comorbidities) or those prioritising improved quality of life as their primary objective. Of note, Abdallah et al additionally affirmed that their study outcomes offer reassurance for patients undergoing PCI along with contemporary medical treatment with regard to the advantages in their quality of life, which are generally on par with those observed with CABG, especially among diabetic patients experiencing less severe angina symptoms43.
Conclusions
It is important to note that the findings of the FREEDOM trial have been influential in significantly shaping the clinical practice of revascularisation in diabetic patients with MVD. However, continually evolving stent technology, improved patient care, personalised medical therapy approaches, and patient characteristics, including comorbidities and anatomical considerations, may influence treatment decisions and could challenge or refine these recommendations. Researchers and clinicians are thus encouraged to continue to explore and challenge the data in individualised clinical scenarios with new technological advancements in PCI, more potent antiplatelet agents and anti-inflammatory agents, and very aggressive lipid-lowering therapy. In view of these therapeutic advances during the last two decades, since the initiation of the FREEDOM trial, now is an appropriate time to revisit the results of CABG versus PCI in diabetic patients with multivessel disease.
Guest Editor
This paper was guest edited by Davide Capodanno, MD, PhD; A.O.U. Policlinico “G. Rodolico-San Marco”, University of Catania, Catania, Italy
Conflict of interest statement
K. Sudhir has served as chief medical officer of Sahajanand Medical Technologies. The other authors have no conflicts of interest to declare. The Guest Editor reports receiving fees from Terumo.
