Percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI) with coronary artery ectasia and massive thrombus remains technically challenging because standard techniques using balloon angioplasty and stenting are unsuitable for such lesions.
A 73-year-old male patient with diabetes and dyslipidaemia was referred to our hospital with a complaint of persistent chest pain. The initial electrocardiogram showed ST-segment elevation in the II, III and aVF leads. The patient was diagnosed with inferior AMI. An emergency coronary angiography (CAG) revealed that the distal right coronary artery (RCA) was completely occluded with a massive thrombus (Figure 1A). Multiple rounds of thrombus aspiration were performed, but few fibrin thrombi were removed, and Thrombolysis in Myocardial Infarction (TIMI) flow remained grade 1 (Figure 1B). Intravascular ultrasound (IVUS) revealed a markedly positive remodelled ectatic vessel exceeding 8.0 mm, filled with a massive thrombus (Figure 1C). We inserted an intra-aortic balloon pump because the patient developed cardiogenic shock, and attempted to reduce the thrombus using excimer laser coronary atherectomy (ELCA). A 1.4 mm concentric-type laser catheter was passed through the lesion and pulled back at a speed of 1.0 mm/s with an additional injection of saline (initial fluency of 40 mJ/m2, repetition rate of 25 Hz) (Figure 1D, Figure 1E). After the third round at the initial setting, the fluency and repetition rate subsequently increased to 60 mJ/m2 and 40 Hz, respectively. While the floating thrombus remained at the ectatic lesion, TIMI flow grade 3 was achieved (Figure 1F). Additionally, IVUS showed a reduced thrombus (Figure 1G). We finalised the procedure after considering the risk of distal embolism and slow flow/no-reflow phenomenon that could be caused by additional balloon angioplasty or stenting. The patient was treated with 100 mg aspirin and 3.75 mg prasugrel daily and unfractionated heparin (target activated clotting time of 250-300 seconds) for 3 days. Subsequently, the medication was altered to 3.75 mg prasugrel and 10 mg apixaban. A CAG performed on day 6 showed the near disappearance of the thrombus (Figure 1H), and optical frequency domain imaging revealed a slight mural thrombus (Figure 1I). No evident plaque ruptures were observed. At two years, multimodality computed tomography follow-up showed no thrombus (Figure 1J), and the patient was free of cardiovascular events.
Coronary artery ectasia is a strong and independent predictor of the no-reflow phenomenon after primary PCI for AMI1. ELCA is a revascularisation therapy based on the effect of a catheter-guided pulsed ultraviolet excimer laser light, which vaporises the thrombus by emitting photomechanical, photochemical, and photothermal energy2. In addition, exposure to the excimer laser suppresses platelet aggregation and reduces platelet force development capability, which is referred to as the “stunned platelet phenomenon”3. The standard strategy combines ELCA with adjunctive balloon angioplasty or stenting4. In patients with AMI, using ELCA before stenting improves procedural success and reduces in-hospital cardiovascular events5. Although there are limited data on ELCA use during primary PCI, our case suggests that ELCA is feasible for emergent revascularisation in ectatic coronary artery disease with a massive thrombus and favourable midterm durability.
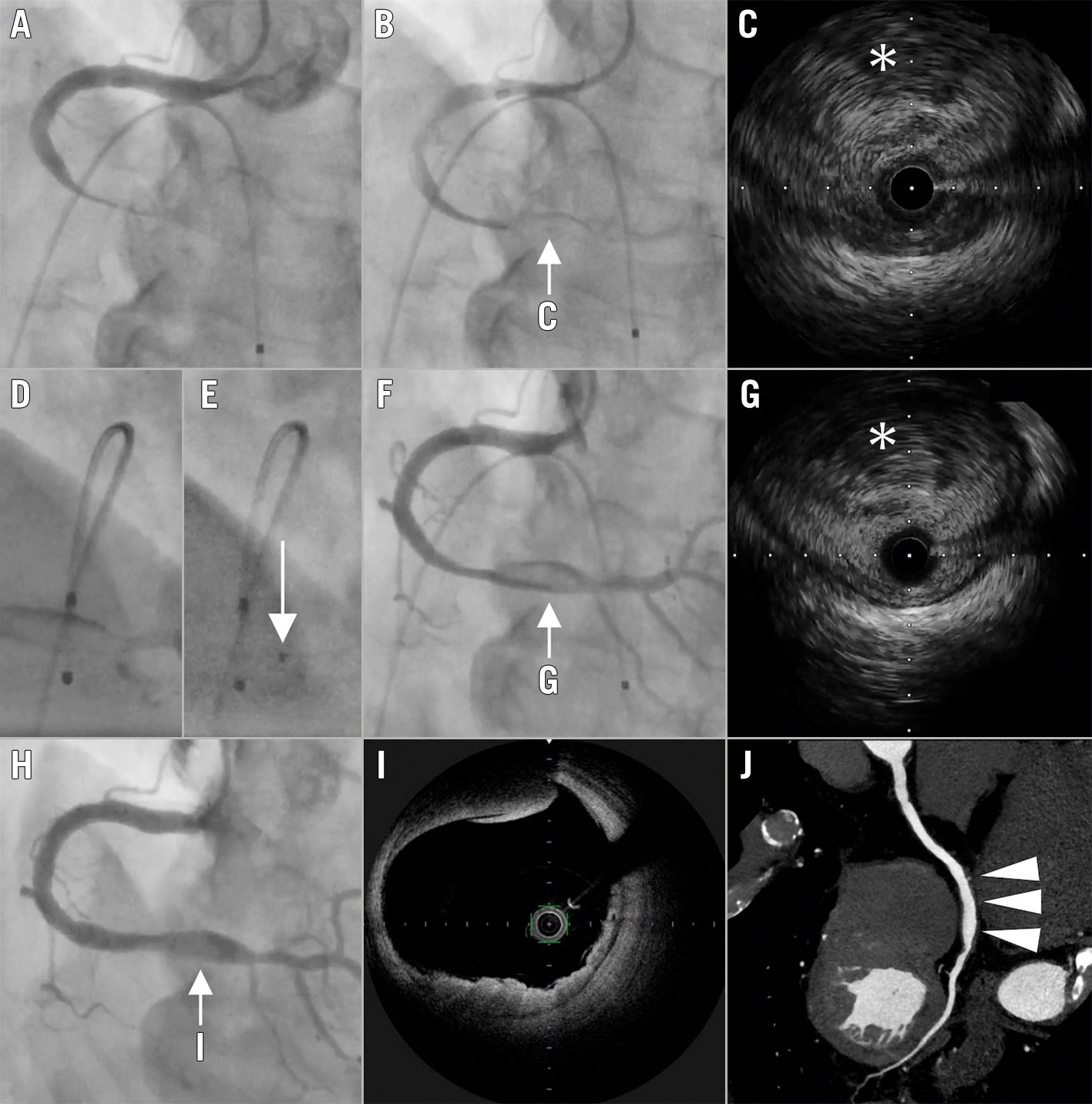
Figure 1. Excimer laser coronary atherectomy for acute myocardial infarction with coronary artery ectasia and massive thrombus. A) The initial coronary angiography (CAG) of the right coronary artery (RCA) showing total occlusion of the distal RCA (left anterior oblique cranial view). B) CAG after thrombus aspiration, showing grade 1 TIMI flow. C) Intravascular ultrasound (IVUS) depicting a massive thrombus (white asterisk). D, E) Angiography during excimer laser coronary atherectomy (ELCA; white arrow, left anterior oblique view). F) CAG after ELCA, showing grade 3 TIMI flow. G) IVUS after ELCA presented a reduction of the thrombus (white asterisk). H) CAG performed on day 6, showing almost complete disappearance of the thrombus. I) Optical frequency domain imaging demonstrating a slight mural thrombus. J) Multimodality computed tomography follow-up at the 2-year mark, showing no thrombus at the ectatic coronary artery (white arrowheads). TIMI: Thrombolysis in Myocardial Infarction
Acknowledgements
The authors wish to thank all the members of the catheterisation room of the Sakakibara Heart Institute.
Conflict of interest statement
M. Nanasato has received a lecture fee from Boston Scientific Japan. The other authors have no conflicts of interest to declare.
