An 85-year-old female with a history of severe symptomatic aortic stenosis, hypertension, stage 2 chronic kidney disease and diabetes mellitus was repeatedly admitted for New York Heart Association Class 4 heart failure symptoms. An echocardiogram demonstrated a left ventricular ejection fraction (LVEF) of 65%, a severely calcified aortic valve (AV) with an area of 0.53 cm2 and a mean gradient (MG) of 74 mmHg. A coronary angiogram showed minor disease. Computed tomography (CT) showed a narrow coronary sinus and sinotubular junction, with a low left coronary height (9.8 mm) and a long left AV leaflet (11.9 mm) with a large calcium deposit at the tip (Figure 1A, Figure 1B). A simulated valve-to-coronary (VTC) distance of 2.4 mm was at risk of left main (LM) obstruction. The Heart Team meeting concluded the patient to be at prohibitive risk for surgical aortic valve replacement (SAVR).
The options of chimney stenting versus Bioprosthetic or Native Aortic Scallop Intentional Laceration to Prevent Iatrogenic Coronary Artery Obstruction (BASILICA) were discussed with the patient, and she opted in the end to proceed with BASILICA transcatheter aortic valve replacement (TAVR). We performed TAVR with native valve BASILICA of the left coronary cusp (LCC). The compromised en-face and side projections of the LCC were predetermined by CT. CT fusion images were obtained to mark the 3 cusps and LM ostium (Figure 1C) to facilitate targeting the puncture site, thus decreasing the need for repeated contrast injection and maximising the effectiveness of BASILICA. The steps for BASILICA TAVR have been described extensively in various publications1; we simplified the technique as follows:
1) We traversed the cusp leaflet with an Astato XS 20 wire (Asahi Intecc) without preloading, with piggybacking to enhance tactile feedback and to ensure a free wire tip.
2) After snaring the Astato wire into the guide, we backloaded the piggyback catheter, leaving a 4 finger-breadth distance (Figure 1D). This replaced the originally described technique in which the preloaded piggyback microcatheter is retracted from the guide catheter after snaring to allow space for a flying-V formation, which increases the lag time from the wire traversing to TAVR deployment and the possibility of inadvertently pulling on the traversed wire. The technique we employed allows for better tactile feedback on whether the traversed wire tip is free, improving safety.
3) We formed a “flying-V” immediately proximal to the piggyback catheter and proceeded with BASILICA in the usual manner.
After LCC laceration and an aortogram confirming the absence of any complication (Figure 1E), a 23 mm SAPIEN S3 (Edwards Lifesciences) valve was implanted (7.6% oversize). The patient developed cardiac tamponade, and pericardiocentesis was performed. An aortogram showed an LCC annular rupture (Figure 1F). Protamine was administered by autotransfusion. However, a rapid recollection persisted, and cardiothoracic surgeons were contacted for possible urgent repair. In view of the patient’s prohibitive surgical risk status, coiling was attempted first.
The LM was engaged, protected with an extra-backup 3.5 guiding catheter. The LCC was engaged with an Amplatz Left 1 guiding catheter (Figure 1G). A total of 9 Cook coils (one 3×170 mm, one 3×140 mm, one 4×70 mm, three 3×30 mm, three 2×30 mm) and 3 target coils (two 6×300 mm, one 4×80 mm) were deployed (Figure 1H, Figure 1I). An aortogram showed no more contrast extravasation. The pericardial drain output was stopped, and the patient was weaned off all inotrope. Intravascular ultrasound confirmed no coil protrusion or leaflet obstruction to the LM. Transesophageal echocardiography showed a resolution of effusion, with normal TAVR valve function and LVEF.
There was minimal output from the pericardial drain overnight. The patient was extubated the next day with no neurological deficit. A CT was performed 4 days postoperatively, showing no contrast extravasation or haematoma at the rupture site (Figure 1J, Figure 1K).
To the best of our knowledge, this was the first reported native valve BASILICA TAVR in Asia. The use of CT fusion images enabled us to more easily identify and target the otherwise fluoroscopically invisible targets, decreasing the need for repeated contrast injection. The use of a modified BASILICA technique also simplified the manoeuvres required, preventing the inadvertent withdrawal of the Astato wire after crossing and avoiding the cumbersome step of retracting the piggyback catheter. We also demonstrated successful salvage of an annular rupture post-TAVR with a coil embolisation.
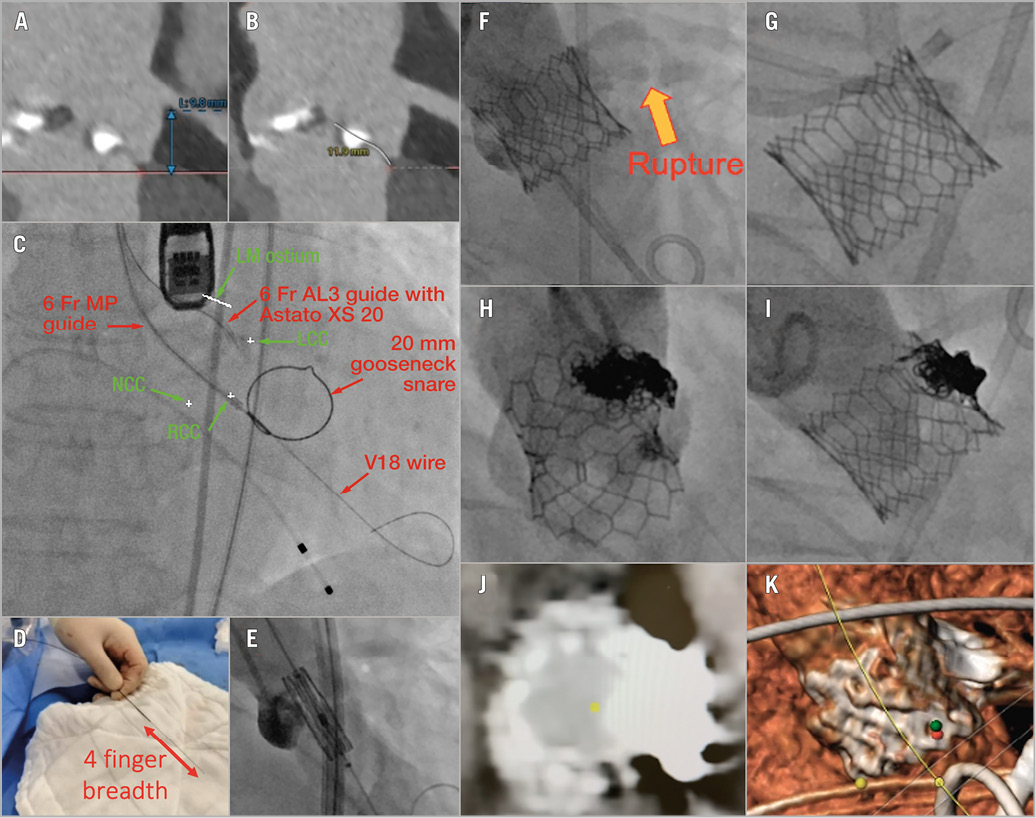
Figure 1. Modified BASILICA TAVR with CT fusion, with coil embolisation for annular rupture. A) Left coronary height. B) Left coronary cusp (LCC) leaflet length. C) BASILICA set-up. D) Backloading of piggyback catheter, leaving a 4 finger-breadth length at the back. E) Aortogram confirming no annular rupture or complication. F) Aortogram showing annular rupture at left coronary cusp. G) Left main engaged with an EBU 3.5 guiding catheter. Left coronary sinus engaged with an AL1 guiding catheter. H) En-face aortogram after coiling. I) Side-projection aortogram after coiling. J) CT confirming no active extravasation or haematoma. K) Post-coiling 3D CT reconstruction. AL1: Amplatz Left 1; BASILICA: Bioprosthetic or Native Aortic Scallop Intentional Laceration to Prevent Iatrogenic Coronary Artery Obstruction; CT: computed tomography; EBU: extra-backup; LM: left main; NCC: non-coronary cusp; TAVR: transcatheter aortic valve replacement; 3D: three-dimensional
Conflict of interest statement
P.A. Villablanca is a consultant for Edwards Lifesciences and Teleflex. The other authors have no conflicts of interest to declare.