A 56-year-old female with hypertension, dyslipidaemia and a family history of premature coronary artery disease presented with exertional dyspnoea. A coronary computed tomographic scan showed a calcium score of 112, moderate stenoses in the mid-left anterior descending (LAD) and mid-left circumflex (LCx) arteries and severe stenosis in the mid-right coronary artery (RCA). We proceeded with coronary angiography (CAG) via the right distal radial artery (DRA). A single puncture of the right DRA was performed without ultrasound guidance. A 5 Fr sheath was inserted, and intra-arterial verapamil, nitroglycerin and heparin were administered. CAG revealed 40% stenoses in the mid-LAD and mid-LCx and a 50% stenosis in the mid-RCA. Hydrophilic sheathless PB3.0 and JR4.0 6.5 Fr guide catheters (Eaucath; Asahi Intecc) were used to perform fractional flow reserve (FFR; with possible angioplasty) of the mid-LAD, mid-LCx and mid-RCA. All FFR values were non-significant. The entire procedure was completed in 45 minutes. There was no radial artery spasm or arm pain. A radial compression band (STEPTY P [Nichiban], which was the only radial compression device available in our institution) was applied and removed after 90 minutes. There was minimal bruising but no haematoma, and she was discharged 4 hours later.
At the 3-week post-procedure review, she complained of pain in the entire right forearm. The distal and proximal radial artery pulses were readily palpable; however, the right forearm was warmer than the left and there was hyperalgesia. Despite the administration of non-steroidal anti-inflammatory drugs (NSAID), her symptoms persisted, and she began to develop mild right-hand weakness. She was referred to a pain specialist 2 weeks later where examination demonstrated allodynia to a camelhair brush and 10g von Frey filament stimuli. Thermography showed an elevated temperature (11°C higher) of the right forearm (Figure 1A) suggestive of complex regional pain syndrome (CRPS) type 1. Pharmacological therapy, with pregabalin and nortriptyline, and hand physiotherapy were commenced. She declined stellate ganglion blockade, which may have provided rapid relief. There was a gradual clinical improvement with a decrease in pain and an increase in hand strength. Repeat thermography at 1 year (Figure 1B) showed a marked reduction of the right forearm temperature (right forearm 0.5°C higher than the left), although she still had minimal residual forearm pain and hand weakness.
Recently, DRA access for CAG and percutaneous coronary intervention (PCI) has been used increasingly. The benefits include a lower incidence of radial artery occlusion and more comfortable ergonomics for patients during PCI1. Several access-site complications have been reported, such as hand haematomas, pseudoaneurysms and radial artery dissection2. Ultrasound-guided access may reduce vascular complications2. CRPS type 1 (previously termed reflex sympathetic dystrophy) or CRPS type 2 (previously known as causalgia) have rarely been reported with conventional transradial access3. Typical symptoms include pain (described as burning, tingling, or stabbing) out of proportion to the initial injury and localised to a distal extremity. There may also be trophic changes and motor dysfunction4. Temperature asymmetry is common, and bedside thermography aids in the diagnosis5. Our patient likely suffered from type 1 CRPS (without nerve injury), whereas type 2 CRPS follows nerve injury with an initial dermatomal pattern. The cause was likely idiopathic in our patient as there was no documented nerve or vascular injury.
The pathophysiology of CRPS is currently thought to be due to an increased sensitisation of the peripheral and central nervous systems with accompanying inflammatory changes and autonomic dysregulation6. There are no reliable predictors of CRPS or methods to prevent CRPS following tissue trauma, although it is more common in females. We believe this is the first reported case of CRPS following an uncomplicated distal radial artery catheterisation. For both types of CRPS, early treatment with NSAID, neuropathic drugs, bisphosphonates, corticosteroids, physical therapy and sympathetic ganglion blockade have been shown to improve outcomes4. Conversely, a delay in treatment worsens the prognosis and may lead to chronic symptoms and disability. Thus, interventional cardiologists should be aware of this debilitating condition that can occur after conventional transradial or distal radial approaches so that early treatment can be instituted.
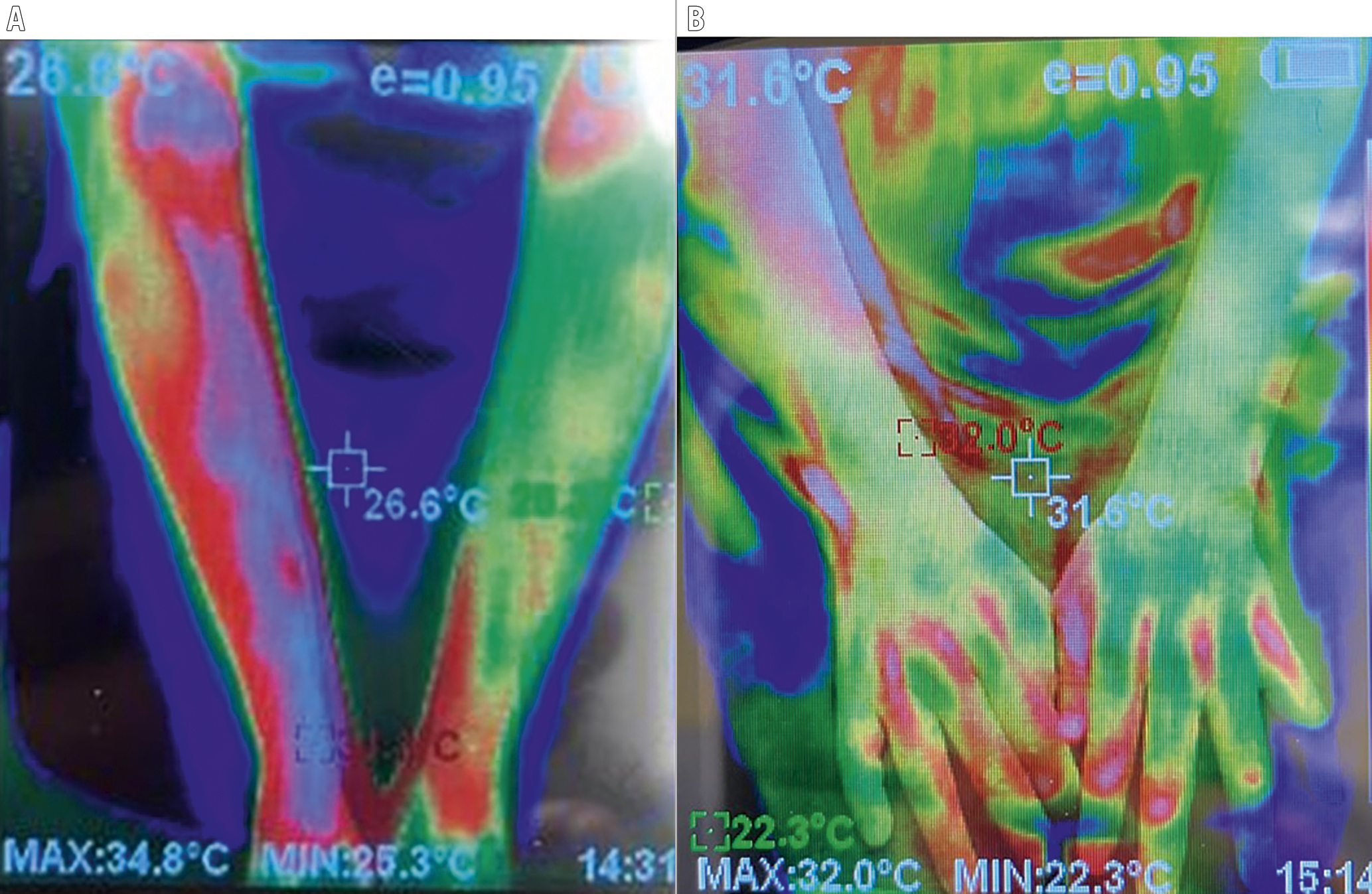
Figure 1. Repeat thermography at presentation and at 1 year. A) Thermogram image at presentation showing an elevated temperature of the right forearm (right forearm 36°C, left forearm 25°C, as estimated by thermography). B) Thermogram image at 1 year showing marked reduction in temperature of the right forearm.
Conflict of interest statement
The authors have no conflicts of interest to declare.
