Introduction
Complete revascularisation (CR) is a desirable objective but may not sometimes be achievable either by percutaneous coronary intervention (PCI) or coronary artery bypass graft surgery (CABG)1,2. Clinical variables including the patient’s age, life expectancy, the severity of symptoms at presentation, associated comorbidities, left ventricular function and myocardial viability are often considered in addition to the extent of disease and complexity of coronary anatomy for deciding the mode of revascularisation in an individual case. The resulting completeness of revascularisation is more often an outcome of the case rather than a choice decision and may affect the long-term outcomes3,4. At times, incomplete revascularisation (IR) may be life-saving, especially in the ST-elevation myocardial infarction setting considering a comprehensive risk-benefit analysis5,6. We aimed to correlate the completeness of revascularisation post PCI with the long-term outcomes in a broad subset of real-world patients with multivessel disease (MVD).
Material and methods
Data of consecutive patients with multivessel coronary artery disease (CAD) undergoing PCI from January 2008 to December 2017 were included in this single-centre, retrospective cohort study. The decision to perform PCI was based largely on the patient’s clinical presentation, lesion characteristics and patient preference, with an aim for CR as far as possible, provided the same could be achieved without a prohibitive risk. Default IR resulted when the operator had planned for a CR procedure but could not achieve the same because of some unexpected intraprocedural difficulties. Elective IR procedures were performed largely in patients with acute coronary syndrome wherein a clear culprit lesion was identifiable and the other vessels or lesions were considered either non-significant or non-amenable to PCI and CABG was not a feasible alternative in that patient for any reason.
A written informed consent was obtained before the procedure from all patients as per the institutional ethics committee approved protocol in accordance with the Declaration of Helsinki7. Unfractionated heparin was given at the time of the procedure and titrated to maintain an activated clotting time (ACT) >250 seconds. Glycoprotein IIb/IIIa inhibitors were given at the discretion of the operator, keeping in mind the complexity of the lesion, stent length, use of multiple stents and the patient’s clinical status. Post PCI, all patients were prescribed dual antiplatelet therapy for a minimum of 12 months along with guideline-directed medical therapy (GDMT) as a policy. All clinical and procedural details were recorded in a pre-specified custom-made software as part of standard departmental protocol, on a day-to-day basis, which provided the database for this analysis. Patients having an active infection, malignancy or bleeding diathesis were excluded from the study.
DEFINITIONS
MVD was defined as the presence of ≥70% luminal diameter stenosis in ≥2 major epicardial arteries. Left main disease was considered significant at a 50% cut-off level. Lesions longer than 10 mm were considered significant at a 60% cut-off level. Patients were stratified into two groups, i.e., “complete revascularisation” (CR) and “incomplete revascularisation” (IR). CR was defined as no vessel with a myocardial value of >1.5 (which equals a proportional myocardial weight of 10% of total myocardial weight as per the modified Greenlane System8,9) and having stenosis of ≥70% being left non-revascularised. IR was defined as at least one or more vessel or a major subdivision with a myocardial value of >1.5 with a stenosis of ≥70% being left non-revascularised for any reason. Procedural success was defined as successful dilatation and recanalisation of at least one major epicardial vessel with stent implantation and residual stenosis of <20% with at least Thrombolysis In Myocardial Infarction (TIMI) grade 2 flow. Cases amounting to procedural failure were excluded from the study. A residual jeopardy score was obtained after multiplying the myocardial value of the vessel or segment left non-revascularised with the grade of stenosis left in that vessel (as per the modified Greenlane System8,9). Patients in whom CR was achieved after two or more staged procedures were included in the CR group only. Procedures were considered staged if performed within the same hospital admission or a stipulated post-discharge period independent of a need generated by a clinical event during the in-between period. The IR group was further sub-categorised and analysed based on a residual jeopardy score as follows: mild IR (residual jeopardy score ≤2.0), moderate IR (residual jeopardy score 2.1-5.0) and severe IR (residual jeopardy score >5.0).
STUDY ENDPOINTS
The primary endpoint of the study was survival free of any major adverse cardiovascular events (MACE) including all-cause mortality, non-fatal myocardial infarction (MI), need for repeat revascularisation (PCI or CABG) and recurrence of or persisting angina of Canadian Cardiovascular Society (CCS) grade 2 or more. Each individual MACE component was considered as a secondary endpoint. Any MI/acute coronary syndrome (ACS) event that resulted in death or a repeat revascularisation was included in the said hard endpoint rather than in the MI or recurrence of angina group to avoid duplication.
FOLLOW-UP PROTOCOL
Follow-up data were obtained at 3 months, 6 months, and then every year as part of a standard follow-up protocol and recorded in the database which had a software-based provision for the same. Incomplete records were refreshed telephonically during the last year of the study period. In each case follow-up was censored at the occurrence of any hard MACE event such as death, non-fatal MI or repeat revascularisation and, in those without a major hard endpoint, time to occurrence of angina was used to censor the follow-up.
STATISTICAL ANALYSIS
Normality of the variables was assessed, and a variable was considered to be normally distributed when the Z-score was within ±3.29. Continuous variables were expressed as mean±standard deviation (SD) or median (interquartile range) and categorical variables were expressed as percentages. An independent samples t-test or the Mann-Whitney U test was used to compare the mean or median values between the groups. The chi-square test was used to test the association between two categorical variables. Kaplan-Meier curves were used to compute cumulative survival of the groups, and the difference in mean and median event-free survival (EFS) time was assessed by log-rank test. Cox regression analysis was employed to evaluate the hazard ratio and 95% confidence limits with corresponding significance levels. A two-tailed p-value of <0.05 was considered statistically significant. The analysis was performed using IBM SPSS statistical software, Version 26.0 (IBM Corp., Armonk, NY, USA) and MedCalc statistical software (MedCalc Software Ltd, Ostend, Belgium).
We used propensity score matching to compensate for the potential selection biases. Propensity scores for incomplete revascularisation were computed using a logistic regression model with the resulting revascularisation as a dependent variable and baseline demographic, clinical and angiographic characteristics as independent variables. The variables entered in the model included ACS presentation, left ventricular ejection fraction (LVEF) <50%, complex lesion intervened and calculated mean stent length per vessel intervened ≥38 mm. We matched each patient with incomplete revascularisation to a subject from the completely revascularised group according to the derived propensity variables with a 1:1 ratio.
Results
A total of 2,960 patients underwent PCI for multivessel CAD during the study period (January 2008 to December 2017). Of these, 362 patients were excluded from the study due to the non-availability of any follow-up data. The remaining 2,598 patients constituted the study cohort. The median follow-up of the study was 54 months with an interquartile range (IQR) of 31 to 84 months (4.5 years; IQR 2.6-7 years). The maximum follow-up was 139 months. Baseline characteristics of all the patients included in the study are summarised in Table 1. CR could be achieved in 1,854 (71.4%) patients while the remaining 744 (28.6%) patients had IR. The two groups had an equal proportion of males, elderly, diabetics, hypertensives, smokers, LV dysfunction (LVEF <50%) and chronic kidney disease (CKD) patients. Distribution of two- and three-vessel disease between the groups was also uniform. However, IR group patients had a higher incidence of ACS (64.1% vs 58.3%; p=0.003), longer mean stent length per vessel intervened (27.9±12.6 mm vs 26.3±11.3 mm; p=0.002) and complex lesion intervention (40.7% vs 29.6%; p<0.0001) including chronic total occlusions (CTO), left main disease and bifurcation lesions. Multi-staged PCI procedures were significantly more frequent with CR as compared to IR. The mean number of stents implanted per patient was significantly higher in the CR group than in the IR group (2.8±0.7 vs 1.86±0.54; p=0.04). IR was therefore, as an outcome, observed more often with sicker patients and in those with more complex lesions intervened.
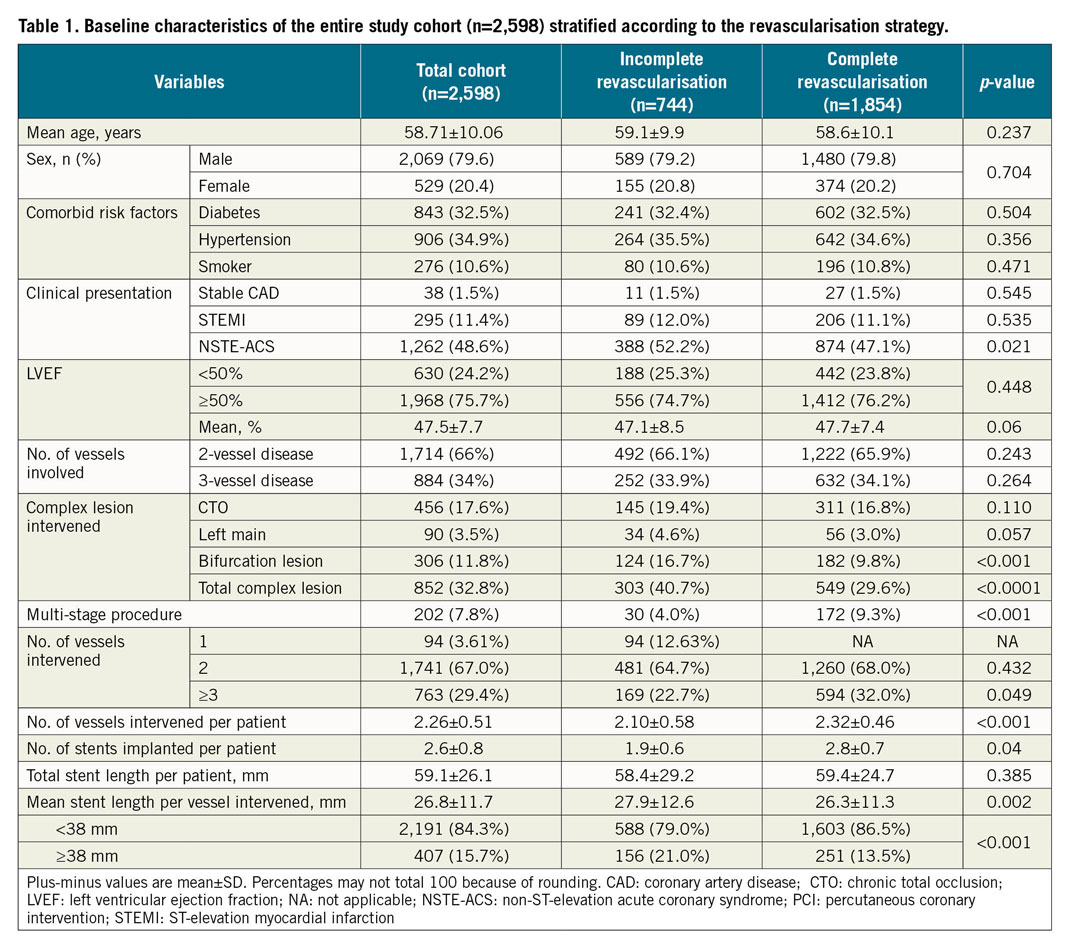
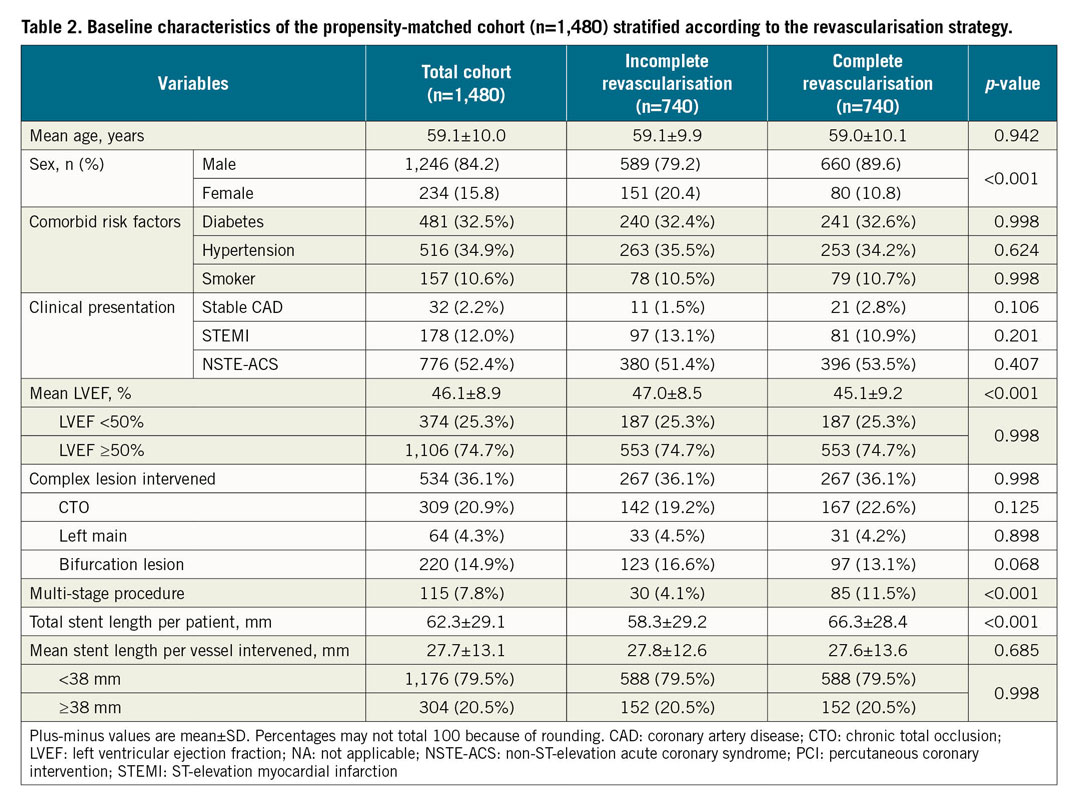
Having identified the significantly different baseline characteristic features between the two groups (CR and IR), a propensity-matched table was derived with 740 matched pairs within the two groups, as shown in Table 2. In the propensity-matched population, there was no difference in the pre-specified outcome deterministic variables in the baseline characteristics.
CLINICAL OUTCOMES
Table 3 shows the clinical outcomes of the study including the primary endpoint of long-term survival free of any MACE, including death, non-fatal MI, need for repeat revascularisation (PCI or CABG) and/or continued angina which was significantly better in the CR group as compared to the IR group (86.4% vs 81.1%; p<0.01), at a median follow-up of 4.5 years (Supplementary Table 1). Among the secondary endpoints, there was no significant difference in the incidence of individual MACE events including all-cause mortality (5.0% vs 3.6%; p=0.153), non-fatal MI (3.5% vs 3.2%; p=0.78), need for repeat revascularisation (10.3% vs 7.8%; p=0.435) and recurrent angina (10.8% vs 9.1%; p=0.066) in the IR and CR groups, respectively (Supplementary Table 2).
Kaplan-Meier survival analysis showed the EFS in the two groups to be better with CR as compared to IR over time (HR 1.52, 95% CI: 1.21-2.02, p<0.01) (Figure 1). Similar curves for individual MACE components including all-cause mortality, repeat revascularisation, non-fatal MI and recurrence of persistent angina are shown in Figure 2A-Figure 2D, with no significant differences shown between the two groups (Supplementary Table 3).
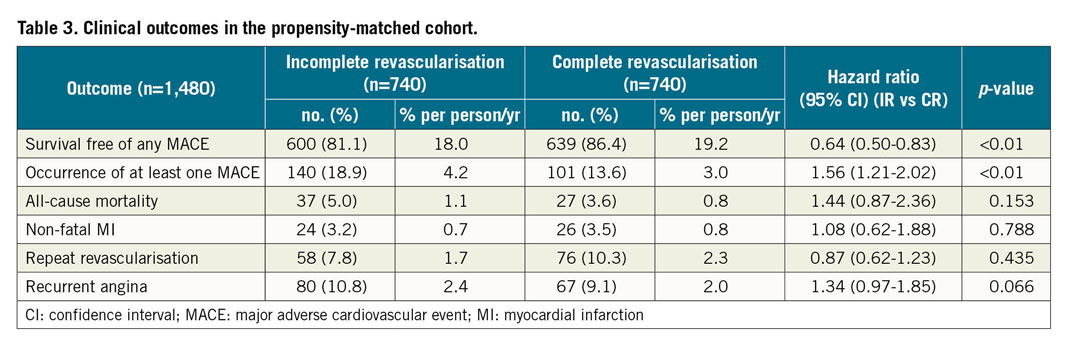
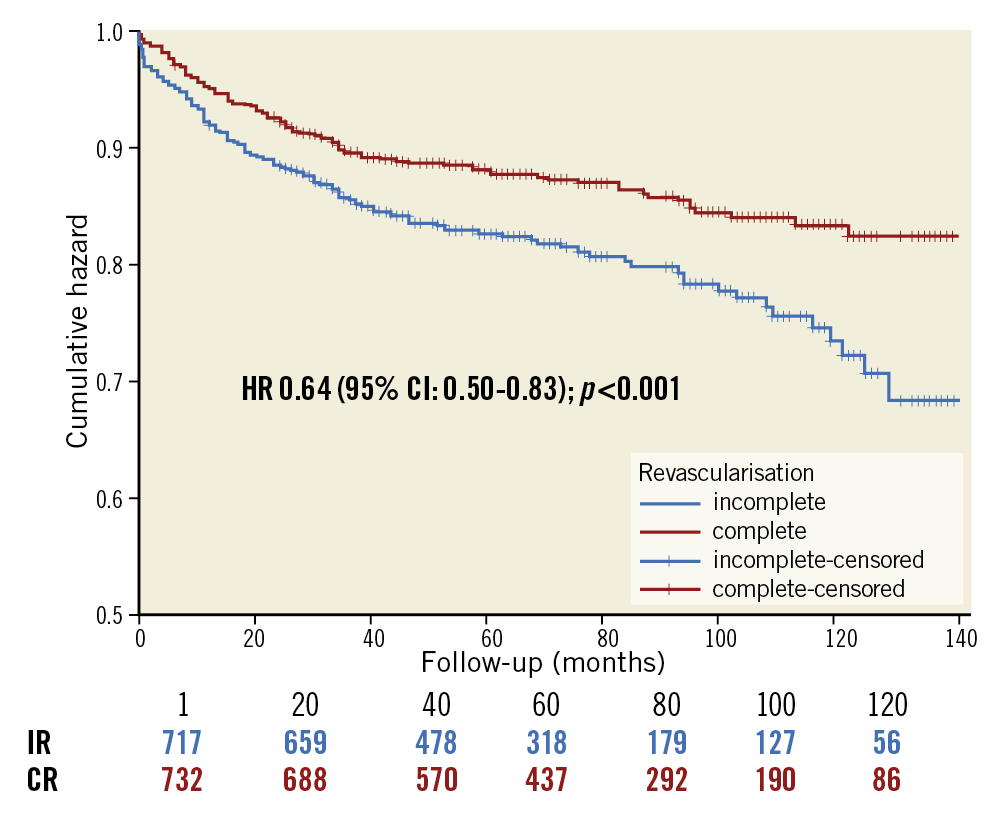
Figure 1. Kaplan-Meier survival curve for multivessel CAD patients treated with DES showing event-free survival of the propensity-matched cohort (n=1,480) with respect to the revascularisation strategy. CAD: coronary artery disease; DES: drug-eluting stent
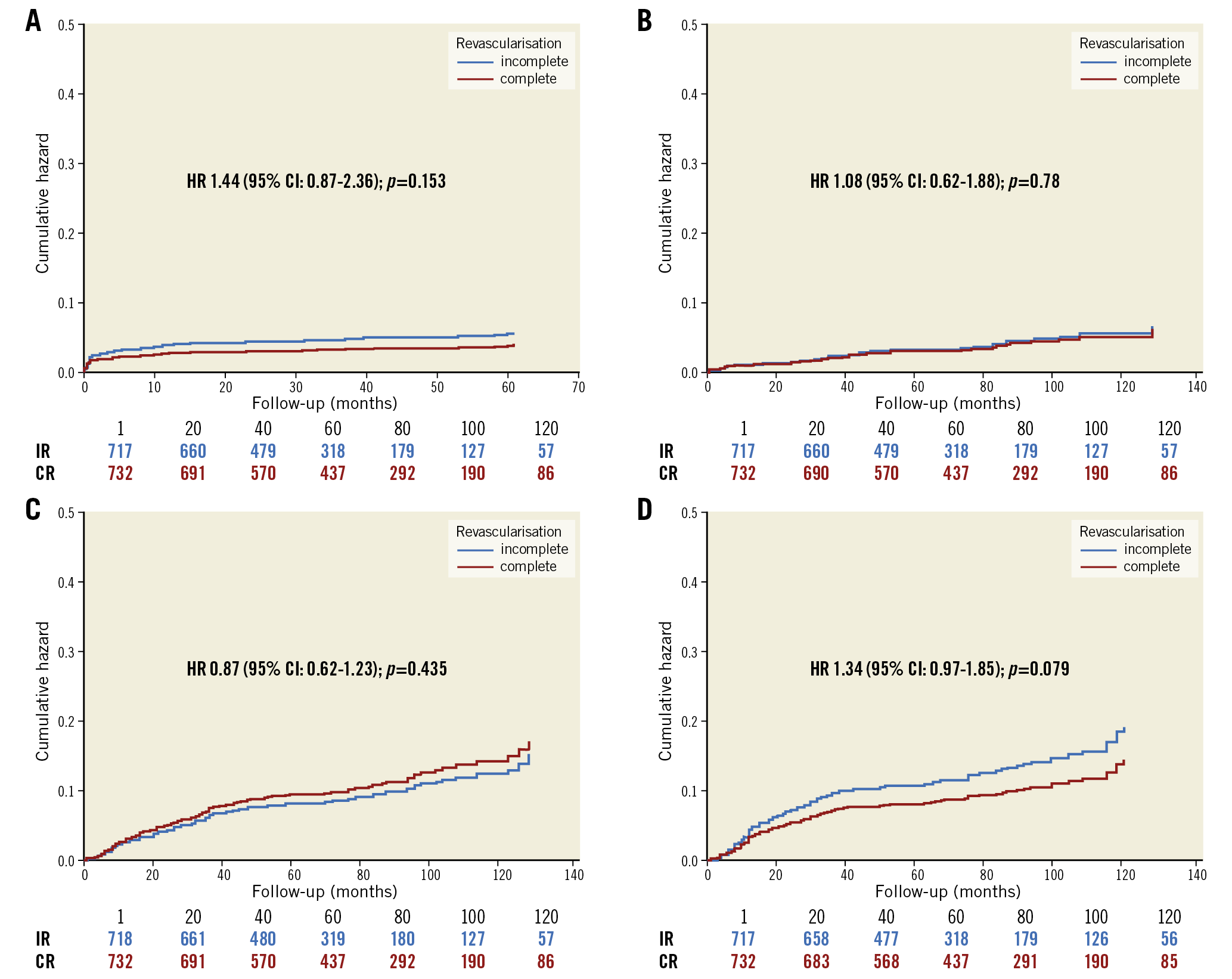
Figure 2. Cox proportional hazard plot in the propensity-matched cohort (n=1,480) showing the cumulative incidence of individual components of MACE. A) All-cause mortality. B) Non-fatal myocardial infarction. C) Repeat revascularisation. D) Recurrent/persistent angina. MACE: major adverse cardiovascular events
Among the incompletely revascularised patients, the residual myocardial jeopardy score was ≤2.0 in 163 (22.0%), 2.1-5.0 in 459 (62.0%) and >5.0 in only 118 (16.0%) patients (Table 4). Figure 3 shows EFS based on the different grades of incomplete revascularisation revealing a significantly worsening EFS rate with the increasing residual jeopardy score. However, the EFS in patients with mild grades of IR was similar to that seen in patients with CR (HR 1.09, 95% CI: 0.68-1.72; p=0.729) (Supplementary Table 4).
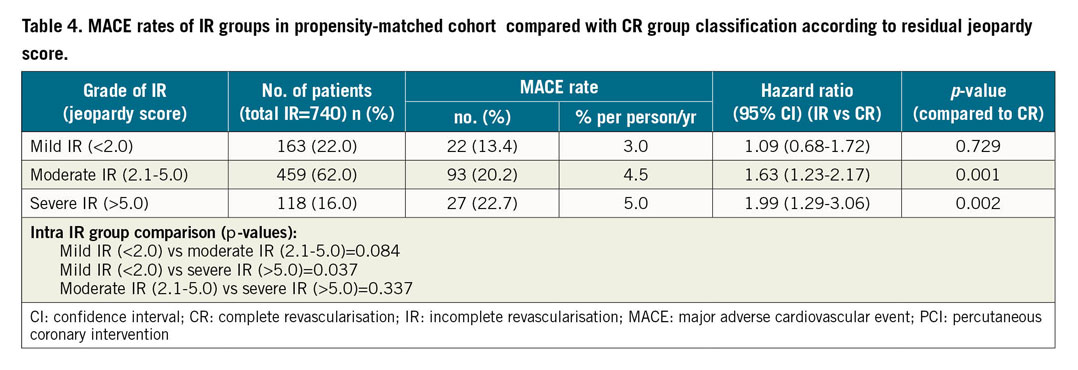
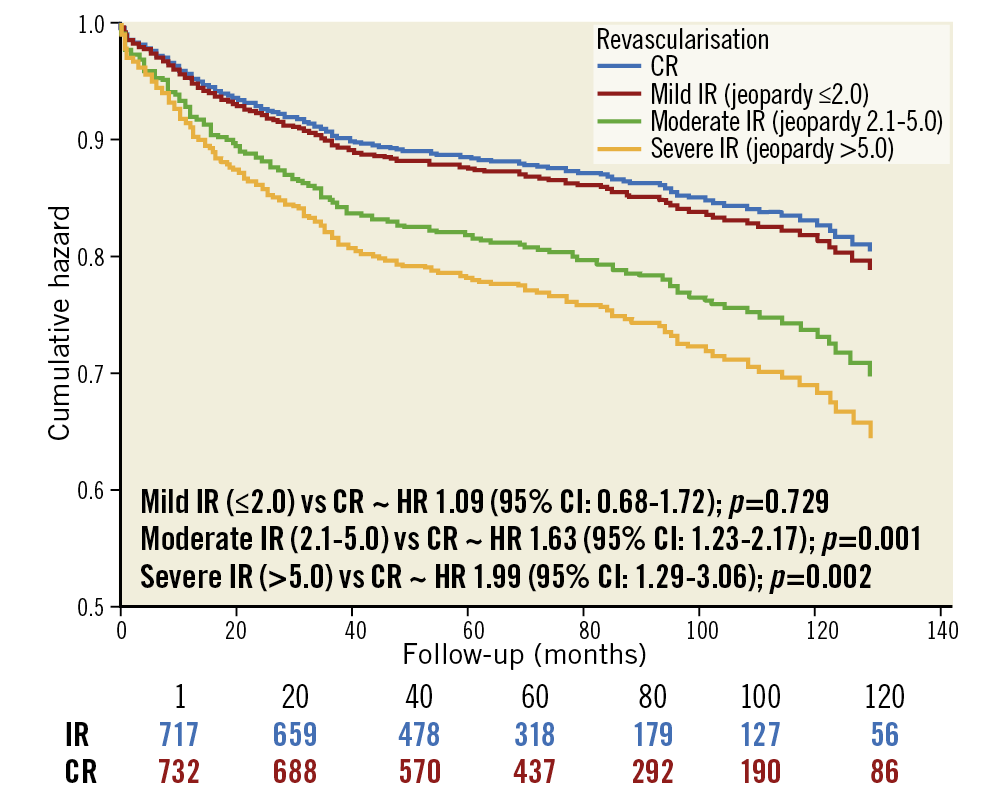
Figure 3. Kaplan-Meier survival curve for multivessel CAD patients treated with DES showing event-free survival of incompletely revascularised patients (n=740) classified according to the residual jeopardy score post PCI as compared to the complete revascularisation strategy. CAD: coronary artery disease; DES: drug-eluting stent; PCI: percutaneous coronary intervention
Discussion
The key observations in our “real-world” study of PCI in MVD in a broad group of patients include, firstly, a better long-term event-free survival free of any MACE including death, non-fatal MI, the need for repeat revascularisation and recurrent or residual angina in the CR group when compared to IR. Secondly, there were no significant differences in the individual MACE components including all-cause mortality, non-fatal MI and the need for repeat revascularisation between the groups. Thirdly, there was a marginally significant higher incidence of recurrent or residual angina in patients with IR. Lastly, there was an absolute survival free of any adverse event in excess of 80% at a median follow-up duration of 4.5 years, even in patients with IR, and survival free of MACE in patients with mild grades of IR (jeopardy score <2.0) was no different from those with CR.
Prior studies have shown conflicting results when evaluating long-term outcomes following complete and incomplete revascularisation in multivessel CAD. Although the majority of data10,11,12,13,14,15,16,17,18,19,20,21 favours CR, there are a few studies which showed that CR alone may not improve long-term clinical outcomes in patients with MVD3,4,22. In a single-centre propensity-matched cohort, Chang et al4 compared outcomes in those with CR versus IR and found that there was no significant difference in the primary outcome of all-cause mortality (8.6% vs 9.0%; HR 1.03, 95% CI: 0.80-1.32, p=0.83), as well as in the secondary outcomes of stroke and repeat revascularisation. Kim et al3 showed that CR alone did not improve long-term outcomes in patients with MVD and hypothesised the need for ischaemia-guided revascularisation.
In a real-world setting, however, CR is something which, although being desirable, may not be achievable even with CABG let alone PCI because of several clinical and anatomical barriers. Gössl et al2 found that CR was achieved in only 57% of patients undergoing PCI as compared to 67% in patients undergoing CABG, highlighting that, although CABG may achieve more CR than PCI, a good proportion are still left with IR with CABG too. In our study, IR was more frequently observed in patients presenting with ACS or in those where complex coronary lesions were intervened or longer stents were used. At times, achieving true CR may mandate intervention in vessels with relatively low myocardial value having complex lesions wherein the effort required may be so high that the risk/benefit ratio may not be in favour. This is supported by our observation that it was only in the presence of moderate to severe IR (jeopardy score >2.0) that total EFS was better with CR than with IR, with almost no difference between those with mild IR and CR. This observation also highlights the importance of objectivising the grade of IR. It can be surmised, then, that mild grades of IR (jeopardy score ≤2.0), as produced by, say, a non-revascularised diagonal, a small obtuse marginal (OM) or a posterior descending artery (PDA) alone, may not be worth the chase if other haemodynamically important vessels have been taken care of. Also, if as an alternative these patients were advised surgery so as to obtain a true CR one still cannot be certain of, firstly, whether CR would always be achieved, especially with these smaller vessels being overlooked by the surgeon too and, secondly, what the true benefit of the same would be, taking into consideration the morbidity of surgery. This further strengthens the importance of a detailed angiographic analysis including an assessment of the myocardial value of each vessel segment being left non-revascularised and the generated residual myocardial jeopardy score that has not been brought out by most prior studies. Our study, however, has brought out this residual jeopardy to its utmost precision by objectively assessing the completeness or incompleteness of revascularisation in each individual case using the modified Greenlane System8,9 of angiographic analysis which includes all these calculations.
Some of the recent data from trials such as COMPLETE23 favours CR as a strategy but this is largely in the acute ST-elevation myocardial infarction (STEMI) setting alone24,25,26,27,28. Moreover, several previous trials6,29 on similar patient subsets have also advocated culprit vessel PCI only as a strategy, which truly is an IR strategy trying to tide over the unstable phase of these sick patients. In several other studies5,30,31, staged revascularisation has been included in culprit vessel PCI or an IR strategy only, which theoretically may not be completely correct because for the long-term outcomes this patient is finally completely revascularised. However, as our study included a broad spectrum of patients, it may be difficult to comment on the impact of completeness of revascularisation specifically in the STEMI subset.
Despite the existing differences observed among various observational studies, large meta-analyses32,33,34,35,36 have suggested a significant benefit of CR over IR, including a relative reduction of approximately 30% in mortality. We, on the other hand, did find a better EFS with a CR strategy but without any difference in mortality outcomes. This could be related to the strict definitions of CR and IR based on our very detailed objective assessment of diagnostic angiograms, including the use of jeopardy scores to classify the degree of IR. Also, the majority (84%) of IR patients had only mild to moderate grades of IR (jeopardy score ≤5.0). A residual jeopardy score in excess of 5.0 (equivalent to about one third of the total myocardial weight being left non-revascularised) was observed in only 16% of the total IR group. This could be because the majority of our patients were accepted with the aim of complete revascularisation except for selected ACS patients where a clear culprit was identifiable and non-culprit vessels were largely non-revascularisable.
Also, ours is a retrospective analysis of recorded patient data rather than a prospective randomised study, with IR being more an outcome than an elective pre-determined strategy. A prospective CR or IR strategy by choice truly may not be possible without a clearly identifiable culprit lesion, as noted in the ACS (STEMI or NSTE-ACS) setting. Also, in day-to-day clinical practice, because CR may not always be achievable and often one may have to accept IR with a certain grade of residual myocardial jeopardy as per the clinical setting, our results could be seen in a different light. That is, despite IR, at least 80% of patients could have a median survival free of MACE of more than 4.5 years and no worsening of mortality outcomes as compared to the CR group. This is an outcome which, in absolute terms, may not be bad at all considering the complexity of the study group patients with nearly 60% having ACS and at least 40% of patients having one or more complex lesions intervened including CTO, bifurcation, or left main, lesion subgroups which were not included in several other trials. A large multicentric prospective randomised clinical trial aiming at IR versus CR while preferable from a methodological standpoint would truly be difficult or nearly impossible to execute except in a STEMI setting.
Study limitations
This being a real-world single-centre study, it could be biased in terms of the criteria considered for revascularisation decision making, which may not be reproducible in other patient populations. Secondly, being an observational study and a retrospective analysis, it may be fraught with all the inherent weaknesses of any such analysis. However, the strength is the meticulous angiographic analysis and prospective recording of data on a day-to-day basis which gives it authenticity. Thirdly, being a single-centre/single primary operator-based study does give it an advantage of uniformity of case types and at least shows what at best or at worst could be possible. Also, documentation of reversible ischaemia was not carried out objectively and decisions were based on clinical judgement alone. Lastly, cerebrovascular stroke and major/minor bleeding events were not included in the study outcome/endpoints which is often done for studies of this type. This was primarily because our software did not have this included as one of the observational endpoints right at the beginning when the software was customised before the study conceptualisation.
Conclusions
In patients with MVD undergoing PCI, complete revascularisation results in better survival free of any adverse event including all-cause mortality, MI, repeat revascularisation or recurrent angina but with no significant difference in any of the individual MACE endpoints.
Impact on daily practiceA selective strategy of incomplete revascularisation could be beneficial in some of the sicker real-world patients with complex multivessel disease wherein, although long-term survival free of all adverse events would possibly be better with complete revascularisation in relative terms, in absolute terms the difference may not be a large one, i.e., a 5.3% difference in total event-free survival over a median follow-up of 4.5 years, and no significant difference in all-cause mortality between the two groups. The difference is driven largely by a marginally significant increased residual angina in the incomplete revascularisation group. |
Acknowledgement
We acknowledge the contribution of Mr Mritunjay Mishra, Research Assistant in the Department of Cardiology, SGPGIMS, for data collection, telephonic follow-ups and documentation of records.
Conflict of interest statement
The authors have no conflicts of interest to declare.
