Introduction
A “minimalist” approach, with an emphasis on optimising pre-, peri- and post-procedural care, has been adopted by many TAVI centres for patients undergoing transcatheter aortic valve replacement (TAVI). While this approach has been shown to be suitable for the majority of patients, there is concern that certain patient characteristics, such as frailty, may not allow for the minimalist approach and early discharge. Indeed, the safety and efficacy of early discharge in frail patients undergoing TAVI is poorly understood1.
We assessed the impact of frailty on early discharge and clinical outcomes using the Vancouver Clinical Pathway in the 3M (Multidisciplinary, Multimodality but Minimalist) TAVR study.
Methods
The 3M TAVR study was a prospective multicentre trial which determined the efficacy, safety and feasibility of next-day discharge in patients undergoing balloon-expandable transfemoral TAVI in low-, medium- and high-volume North American centres2. The Vancouver 3M pathway encompasses minimalist practices and includes standardised pre-, peri- and post-procedural care along with criteria-informed discharge to achieve safe next-day discharge. A composite frailty score was calculated from the five-metre gait speed, hand grip strength and activities of daily living. A composite score was determined, ranging between 0 to 9, the highest score representing the worst frailty. Frailty was dichotomised at the median frailty score (>3), classifying patients as frail and non-frail. Patients with incomplete frailty information were excluded.
Results
A total of 319 of 411 patients were included, with 166 (52%) non-frail and 153 (48%) frail patients. Frail patients were more likely to be older (84.0 vs 83.0 years; p=0.009), had a higher Society of Thoracic Surgeons score (5.6 vs 4.4; p<0.001), and used a mobility aid more frequently (40% vs 16.3%), compared to non-frail patients. There was no significant difference between frail versus non-frail patients for adjusted outcomes of discharge within 48 hours (90.1% vs 94.5%; p=0.64), cardiac readmissions (7.4% vs 5.3%; p=0.59), all-cause readmissions (12.2% vs 7.8%; p=0.72) or a composite of all-cause mortality and stroke at 30 days (3.3% vs 3.0%; p=0.57) (Figure 1).
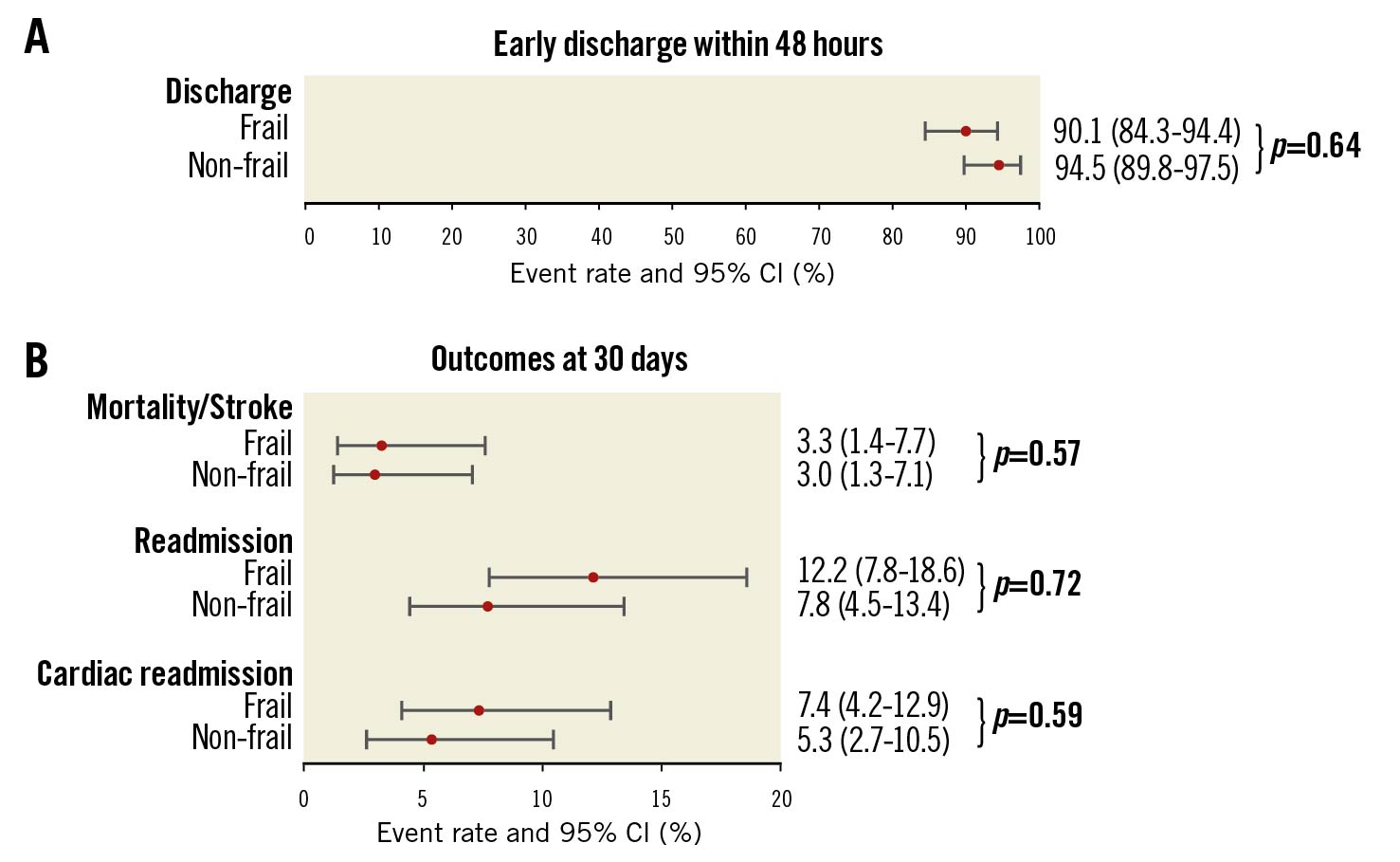
Figure 1. Impact of frailty status on early discharge and clinical outcomes. A) Discharge within 48 hours. Proportions were reported with a p-value from logistic regression, adjusting for diabetes mellitus. B) Outcomes at 30 days. Kaplan-Meier based event rates were reported with p-values from Cox models. Composite of all-cause mortality and stroke was adjusted for device type, and cardiac readmission was adjusted for the pre-mean gradient. No significant confounder was identified for the all-cause readmission. CI: confidence interval
Discussion
This study demonstrates that a clinical care pathway with a rapid return to baseline function and early discharge to the patients’ usual living conditions can be achieved safely in frail patients undergoing TAVI.
Frail patients are at risk of geriatric issues such as delirium, urinary retention, dehydration and malnutrition. Delaying discharge may accelerate functional deconditioning3. Frailty may put patients at risk for readmission and thus preclude early discharge. Conversely, given their risk for deconditioning and adverse events from hospitalisation, a minimalist approach with an emphasis on a rapid return to baseline function and early discharge to their usual living situation may be the most advantageous approach for frail patients undergoing TAVI.
Society faces an unprecedented challenge to overcome the COVID-19 pandemic. Essential TAVI services must be provided for patients at high risk for cardiovascular events in the short term, while still acknowledging the need to focus the majority of healthcare resources on the pandemic. A minimalist approach to TAVI that ensures patient safety without utilising crucial critical care infrastructure may once have been desirable; however, it is now of increasing importance. In frail patients, this may be of particular importance.
Limitations
Our study has important limitations. The study was not randomised, and despite adjustment, results may have been influenced by selection bias. There may have been insufficient power to determine a difference based on frailty. A number of frailty scores exist, and an alternative score may have impacted the identification of frailty in this study. However similar composite frailty scores have been used in prior publications and been shown to be a good discriminator of frailty4.
Conclusions
Frail patients undergoing TAVI with a minimalist approach had similar clinical outcomes and early discharge compared to non-frail patients. A clinical care pathway with an emphasis on a rapid mobilisation and a return to baseline function and the patients’ usual living situation can be safely used with excellent clinical outcomes for frail patients undergoing TAVI.
Conflict of interest statement
S. B. Lauck is a consultant to Edwards Lifesciences and Abbott. J. Sathananthan is a consultant to Edwards Lifesciences and Medtronic. H. C. Wijeysundera receives research funding from Edwards Lifesciences and Medtronic. J. G. Webb is a consultant to, and has received research funding from, Edwards Lifesciences, Abbott, and ViVitro Labs. D. Wood is a consultant to, and has received research funding from, Edwards Lifesciences and Abbott. The other authors have no conflicts of interest to declare.

