Currently, the use of a drug-coated balloon (DCB)-only approach to percutaneous coronary intervention (PCI) is expanding, as seen by the number of publications, ongoing randomised controlled trials (RCTs) and sessions at major global interventional meetings. The concept of less metal long term is one of the driving forces behind this move, as demonstrated by Shin et al in their paper reporting a reduction in events with reduced drug-eluting stents (DES) and increased DCB in multivessel procedures1. A closely related issue of reduced DES implantation is addressed in this edition of AsiaIntervention by Teo et al in a retrospective analysis of the hybrid approach to PCI2. This term describes the combination of DES and DCB within the same vessel or bifurcation. The report covers a one-year period identifying 401 patients, of whom 363 patients had 12-month follow-up data. Their results are impressive with target lesion failure (TLF) of 2.2% (target vessel myocardial infarction [TVMI] 0.83%, ischaemia-driven target lesion revascularisation [ID-TLR] 0.83% and cardiac death 0.55%). The majority of DCBs were paclitaxel-based, whilst the DES were -limus-based. Concern over mixing -limus and paclitaxel is addressed and is shown to be safe at one year. DES were bigger in diameter and length than DCBs, suggesting that more proximal lesions and the main branch (MB) of bifurcations were the intended DES recipients, with DCBs presumably used distally and in the side branch (SB). Bifurcation PCI was reported in 19% of cases. The case mix was 80.8% elective but complex with 72% type C, very long lesions, and 60% with diabetes. Intravascular imaging (IVI) was used in 30% of cases and calcium modification in 5%. This is an impressive and detailed publication from a respected high-volume centre performing complex PCI and adds to the data supporting the move away from a complete DES approach to PCI.
One of the major concerns with this approach is the safety aspect of a proximal DES relying on a balloon-only outflow, raising the possibility of edge dissections and acute vessel closure. The excellent safety data of Teo et al2, however, give operators reassurance that a meticulous approach to lesion preparation and assessment of the acute balloon result will allow a successful PCI. The use of IVI in 30% of cases is interesting, but it is not clear if this represents IVI use in guiding lesion preparation, DES optimisation, or assessment of DCB preparation and acute results. We would not recommend the use of IVI in a DCB-only approach for the following reasons: inexperienced operators may bailout to DES on seeing multiple luminal dissections; DCB-only PCI results are based on angiographic vessel sizing of 1:1, but IVI will increase device size and thus increase the use of bailout further; IVI tends to promote the treatment of longer lesions, whilst a DCB-only approach is more minimalist and forgiving. However, the ULTIMATE-III trial supports more aggressive lesion preparation with balloons that are 0.25 mm larger when IVUS-guided rather than angiographically guided, with less late lumen loss but a higher bailout rate3. Similarly, in the TRANSFORM I study, a reduction in angiographical late luminal loss was seen for the paclitaxel DCB with increasing dissection volume4. The old axiom of gain associated with loss seems to no longer apply, rather now, “the more you gain, the more you get” when using paclitaxel-coated DCB5.
A major deficiency of real-world cohort publications is the lack of understanding of the initially intended PCI technique, so we do not know how often the final hybrid result was the primary intention or was driven by bailout in more proximal larger vessels due to unsuccessful optimal lesion preparation or a vessel-threatening dissection. We encourage a full DCB-only approach to such long lesions where possible but in the knowledge that the hybrid approach is possible.
Bifurcation PCI is important, but we feel that in this paper it is a distraction. We suggest the simplest approach would be DCB-only for all lesions. The hybrid approach is required in only 2 situations. Firstly, when there is a planned DCB to the SB but elective or bailout DES to the MB. SB lesion preparation and DCB are performed before MB DES implantation. The stent does not then need to be recrossed (a more attractive hybrid option), but post-dilatation and potting is advised. Secondly, when MB DES is elective or bailout, but the SB was not an intended target but requires rescue after MB DES implantation. After a good balloon result is achieved, this is the only scenario in which we advocate a DCB through a newly implanted DES. Kissing and potting, as necessary, should be performed. The problems with this latter approach are increased complexity, reduced DES integrity, and the theoretical problem of drug accumulation at the ostium of the SB in the vicinity of new bare DES struts. Figure 1 illustrates the different concepts of bifurcation treatment including DCB.
In conclusion, we congratulate Teo et al2 on adding to the data suggesting a reduction in DES use is safe and efficacious and encourage operators to bear such data in mind in their daily practice. The results of large landmark RCTs will hopefully promote the DCB-only approach over the next few years.
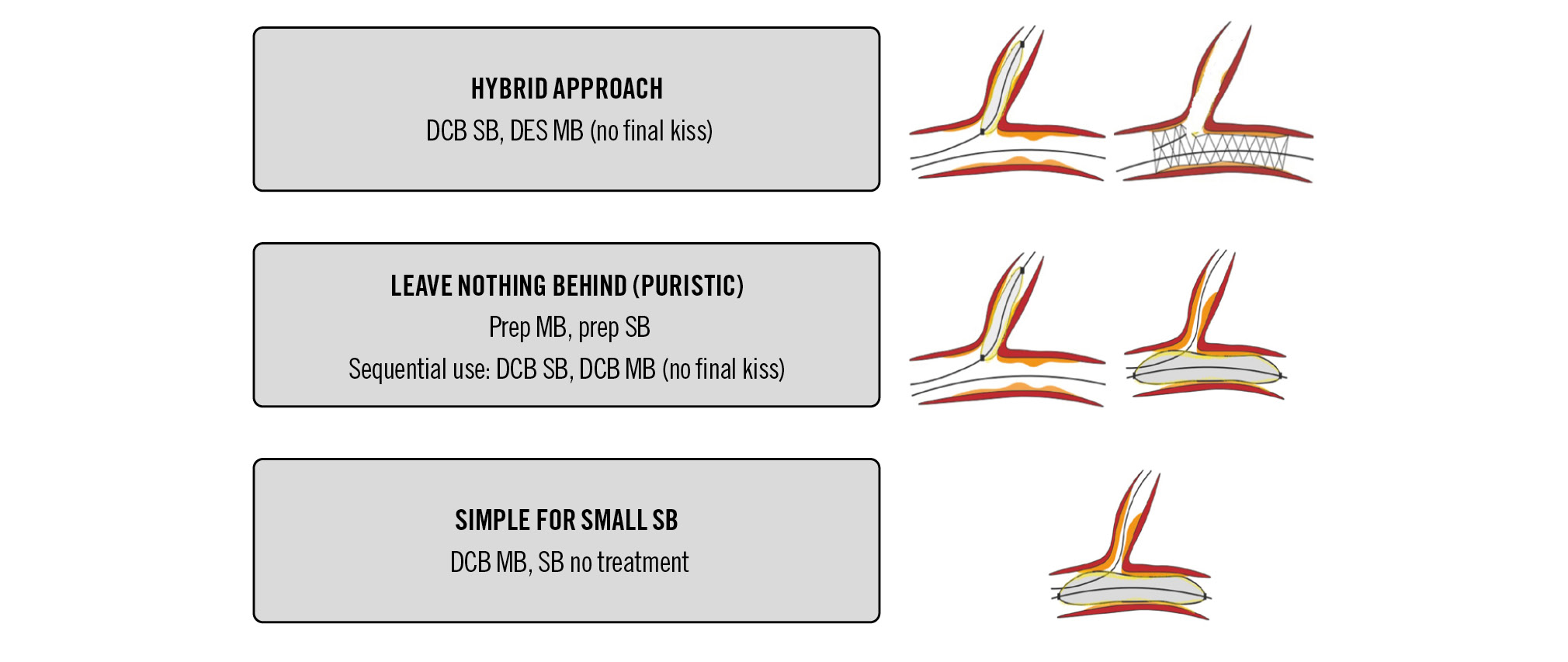
Figure 1. Different scenarios of DCB treatment in coronary bifurcations. DCB: drug-coated balloon; DES: drug-eluting stent; MB: main branch; SB: side branch
Conflict of interest statement
S. Eccleshall received research grants for investigator-initiated research and lecture honoraria from B. Braun. He is a shareholder of MedAlliance and also acts as a consultant for B. Braun, Cordis, Medtronic, and MedAlliance. B. Scheller is a shareholder of InnoRa GmbH and received lecture fees and consulting honoraria from B.Braun and Medtronic.
