The fractal geometry of coronary bifurcations defines a relevant diameter mismatch between the proximal main branch (MB) and its daughter branches. One common step in every bifurcation percutaneous coronary intervention (PCI) is the proximal optimisation technique (POT) which has several advantages1 including prevention of stent distortion. An observation by Matsuda et al suggested that a malapposed stent segment (arc of >180 degrees) can expand freely in the axial dimension, while in the case of apposed but underexpanded stents, less elongation is expected once postdilated2. This is very relevant in left main interventions, as stent elongation can result in clinically relevant pitfalls like dynamic protrusion of stent struts into the aorta which, in turn, creates a risk of strut damage by the guiding catheter as well as difficulties with ostial catheter engagement and wiring for reinterventions. The European Bifurcation Club recommends starting the POT at the carina3. We sought to investigate and compare the stent length if we start the POT from the most proximal end of the MB stent and then move towards the carina (modified POT) versus the traditional POT in a bifurcation model.
Traditional and modified POT were simulated in a silicone bench model. The bench model had a proximal segment (representing the proximal MB) with a 5.00 mm inner lumen diameter and a relatively long length (longer than the POT balloon). A short transition zone of 1.00 mm in length connected the proximal segment with two distal segments (representing the distal MB and the side branch) with an inner lumen diameter of 3.50 mm each. Stent deformation during POT was tested with 3.50×28 mm stent platforms in three different designs (Abbott, Boston Scientific, Terumo). Stents were first deployed with nominal pressure, with the predefined POT segment length protruding into the proximal MB. This was followed by POT. Only non-compliant balloons were used for POT at nominal pressure. In simulating the traditional POT, the balloon was positioned with its distal marker at the proximal end of the transition zone, simulating the level of the carina, while in the modified POT, the balloon was positioned with its proximal marker at the proximal edge of the stent strut and continued toward the carina. The stent length after the final POT was measured using a handheld calliper device. The procedure was repeated 3 times for each stent platform (for a total of 9 stents). There was significant lengthening of the stent when the conventional POT technique was used (Figure 1A, Moving image 1), when compared to the modified POT technique (30.72±0.19 mm vs 28.45±0.11 mm; n=9 stents) (Figure 1B, Moving image 2). Stent elongation after traditional POT may be due to two mechanisms: the majority may be due to overexpansion, with a tight “balloon-to-strut” interaction stretching the crowns and connectors longitudinally; the other may be the POT balloon sliding backwards during the opening and pulling the stent struts back from the distal MB. The second mechanism is only likely if the stent is undersized compared to the distal vessel diameter1. After modified POT, struts of the proximal MB stent are well apposed, thereby creating axial resistance to stent elongation. A jailed wire in the side branch with malapposed struts in the left main increases the risk of longitudinal stent deformation when an attempt is made to pull the POT balloon from the carina towards the proximal part, which can be avoided with the modified POT.
These findings require further confirmation with bench testing and imaging evaluations, and they need to be replicated in a large number of clinical cases.
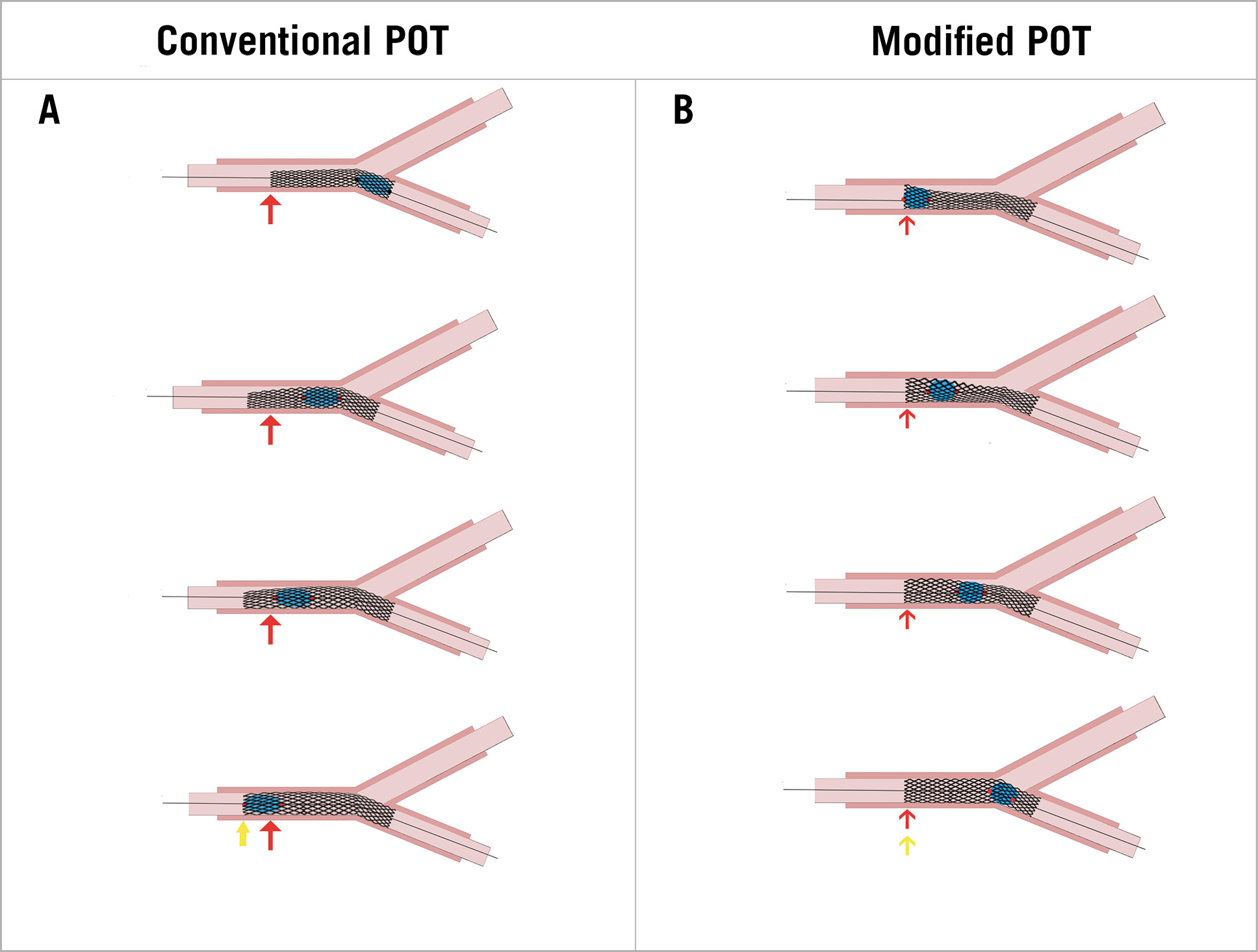
Figure 1. Conventional vs modified POT. A) The conventional proximal optimisation technique (POT) is associated with stent elongation. B) The modified proximal optimisation technique is not associated with significant stent elongation.
Conflict of interest statement
The authors have no conflicts of interest to declare.