Coronary angiography was indicated for a 66-year-old female patient with a history of diabetes mellitus, dyslipidaemia and hypertension who underwent myocardial revascularisation in 2014 (left internal mammary artery [LIMA] to left anterior descending artery [LAD] and saphenous vein grafts [SVGs] to the right coronary artery [RCA] and the first obtuse marginal branch [OM]). She complained of progressive chest pain and effort dyspnoea. Her stress test was positive, and her myocardial scintigraphy showed anteroseptal ischaemia.
Angiography, performed using right femoral artery access, demonstrated chronic occlusion of the distal left main (Moving image 1), patency of both SVGs (Moving image 2, Moving image 3), no collateral vessels to the LAD and normal left ventricular (LV) function. An aortogram showed a calcified ostial occlusion of the left subclavian artery (LSA) (Moving image 4). Considering that LV function was normal and that there were no collaterals to the LAD, the LIMA-to-LAD was considered to be patent. However, since the LSA was chronically occluded proximally, with no visible collateralisation, LIMA flow could only come from the vertebral system. Hence, an angiography of the right vertebral artery (VA) was performed. It demonstrated a widely patent vessel that provided a good retrograde flow to the left VA, which had a 90% ostial stenosis (Moving image 5, Figure 1). A later Doppler ultrasound examination performed on the ward confirmed inverted flow in the left vertebral artery, compatible with subclavian steal physiology. Selective LIMA-to-LAD angiography performed by left radial artery access showed a good functioning graft, with no significant stenoses in either vessels (Moving image 6).
Although a percutaneous recanalisation of the chronically occluded LSA would naturally be the first therapeutic choice for a case like this, this procedure was considered very challenging in this specific patient, as there was no proximal tapered stump, and the occluded segment (as demonstrated by the angiography done by left radial access) was long and calcified. Angioplasty of the ostial left VA could also potentially alleviate myocardial ischaemia, but it would probably lead to subclavian steal symptoms. Therefore, a left common carotid-to-LSA bypass was proposed as a therapeutic strategy. However, despite a full explanation of the clinical picture, the patient declined any further invasive procedure.
Patients with subclavian steal syndrome are frequently asymptomatic1. Cardiac ischaemia, however, may occur in patients revascularised with mammary artery grafts while using their ipsilateral arm. In this case, the concomitant left ostial VA stenosis prevented subclavian steal symptoms but impaired flow to the LSA and LIMA, leading to myocardial ischaemia. The case of this patient underscores the need to look for symptoms of vertebrobasilar insufficiency and for interarm blood pressure differences in patients with myocardial ischaemia after surgical revascularisation that used one or both internal mammary arteries.
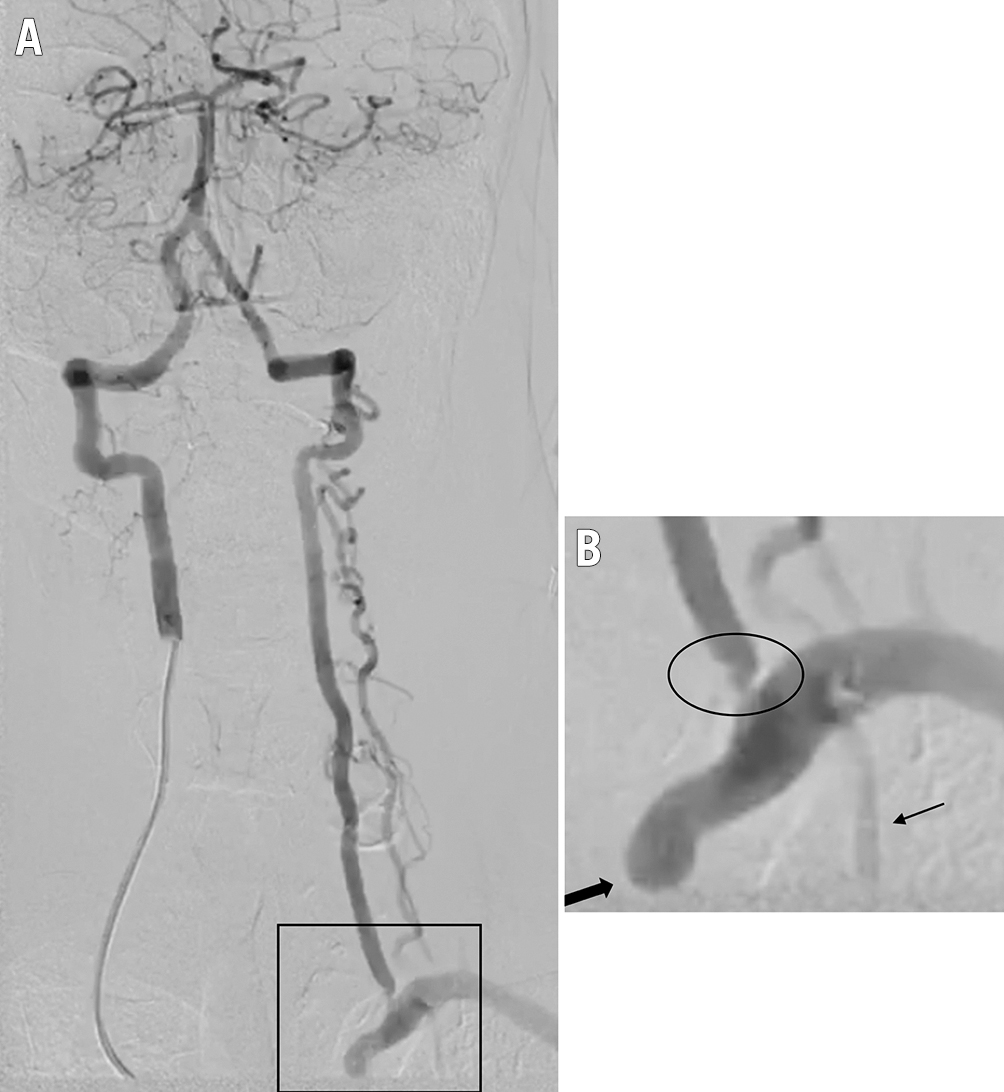
Figure 1. Right vertebral artery angiography. A) Contrast injection in the right vertebral artery shows retrograde flow of left vertebral artery supplying the left subclavian artery and left internal mammary artery (LIMA). B) Magnification depicts the left subclavian artery ostial occlusion (thick arrow), LIMA (thin arrow) and ostial left vertebral artery stenosis (circle).
Conflict of interest statement
The authors have no conflicts of interest to declare.

