An 85-year-old woman was referred to our hospital with severely symptomatic mitral regurgitation (MR). Transoesophageal echocardiography (TOE) showed a small mitral valve (MV) area (MVA) (2.21 cm2 on three-dimensional multiplanar reconstruction); mean MV pressure gradient (MVPG) of 1 mmHg, with restricted anterior mitral leaflet (AML) motion due to rheumatic changes, and MR jet from the A2/P2 region (Figure 1A–Figure 1C, Moving image 1, Moving image 2). Despite the rheumatic MV anatomy, our Heart Team offered transcatheter edge-to-edge repair because of the patient’s frailty and high surgical risk.
The procedure was performed on day 6 after admission. The MitraClip G4 NT (Abbott) was selected, and full grasping of the A2/P2 central region demonstrated worsened MR with unacceptably elevated MVPG (14 mmHg) and reduced MVA (0.43+0.35 cm2) (Figure 1D–Figure 1F, Moving image 3, Moving image 4). The target region was changed to the medial area of A2/P2, and full grasping showed a significant reduction of MR from 4+ to 2+, with acceptable MVPG (4 mmHg) and MVA (1.11+0.27 cm2) (Figure 1G–Figure 1I, Moving image 5, Moving image 6). The MitraClip was finally implanted without any complications. Thereafter, the patient was discharged on postoperative day 6 with reduced dyspnoea. One month after the procedure, the transthoracic echocardiography showed no evidence of MV damage, and the MR was reduced to 1+ with mildly elevated MVMG (8 mmHg). The patient was in a good condition and had no heart failure exacerbations during the 6-month follow-up.
Although the latest generation of MitraClip G4 NT was used in this case, it made no difference to the treatment quality because the clip size was the same as that of former generations. Central MitraClip implantation in the A2/P2 region is favoured over the paracentral position to prevent clinically relevant mitral stenosis1. As the AML is longest in the centre, implantation here yields lower valve tension and greater stability. However, owing to the reduced AML flexibility in rheumatic MVs, central implantation may unacceptably increase the MV tension, resulting in failed MR reduction and elevated MVPG due to significant residual MR, together with smaller neo-MVA. In contrast, A2/P2 paracentral implantation may stabilise the leaflet coaptation without excessively increasing the valve tension and MVPG, as it preserves the lateral AML motion. This technique provides a larger MVA and more MR reduction than central implantation. While a rheumatic MV anatomy is generally considered a relative contraindication, the paracentral implantation technique may be useful to avoid clinically significant mitral stenosis when a MitraClip is necessary.
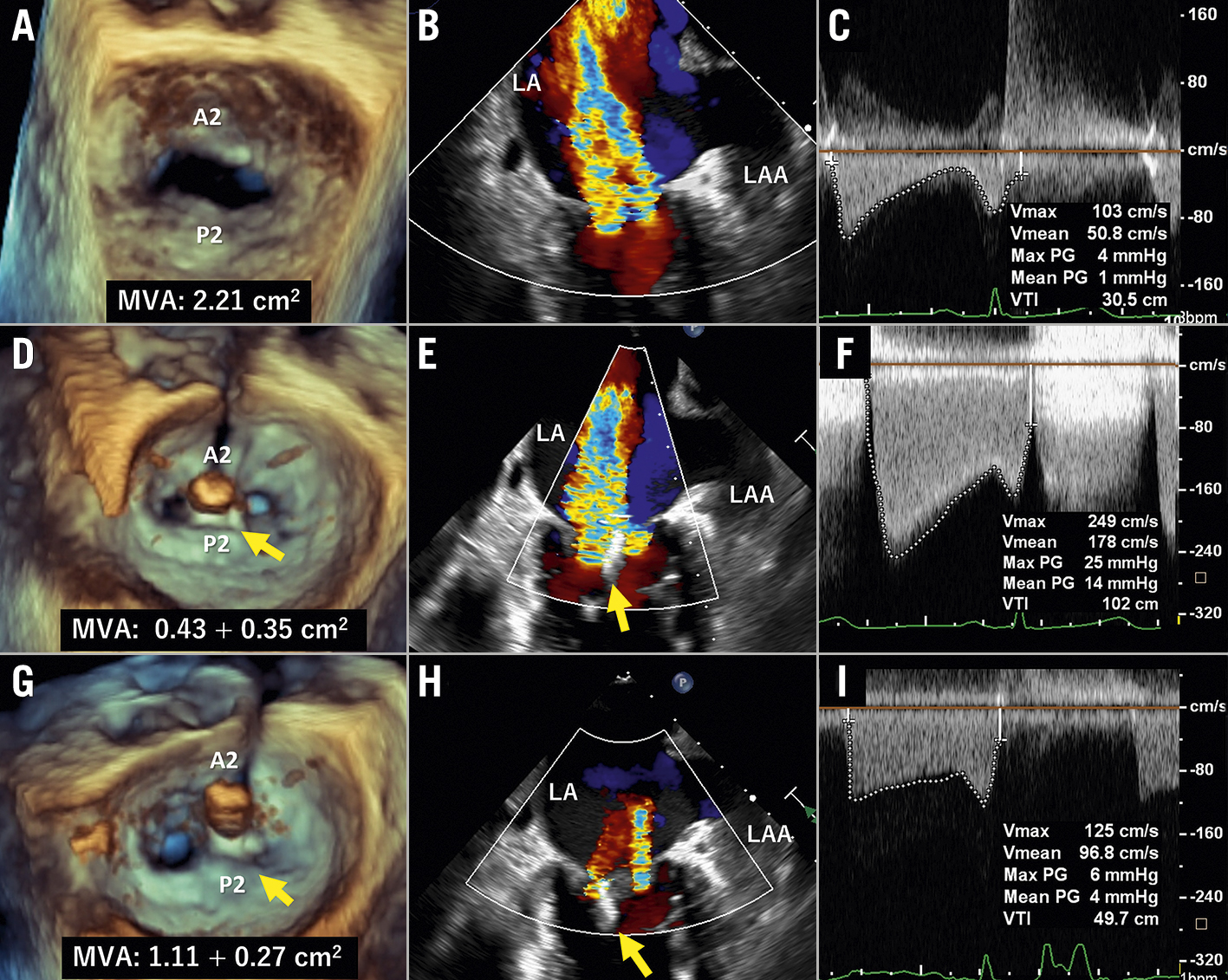
Figure 1. Transoesophageal echocardiography images at screening and during the procedure. En face commissure, and mitral valve pressure gradient images, at screening (A-C) and during the procedure after the central (D-F) and paracentral full grasping (G-I). Yellow arrows indicate the MitraClip. LA: left atrium; LAA: left atrial appendage; MVA: mitral valve area
Conflict of interest statement
A. Kataoka and Y. Watanabe received remuneration from Abbott Medical Japan as proctors for MitraClip. The other authors have no conflicts of interest to declare.
