Introduction
Occupational radiation exposure is a major concern for cardiac catheterisation laboratory workers. Despite improvements in radiation safety, many cardiologists are unfamiliar with radiation biology and the cumulative nature of the risks of ionising radiation. Radiation in the catheterisation laboratory is generated using either fluoroscopy or cineangiography. Fluoroscopy, which is required for most of the procedural time, causes ~40% of the total radiation exposure to staff and patients, while cineangiography contributes ~60% of the total radiation exposure1.
Percutaneous coronary intervention (PCI) procedures can result in 10-fold higher radiation compared to diagnostic catheterisation, and an average PCI procedure results in 150 times more exposure than a chest radiograph and 5 times the annual radiation exposure received as environmental background radiation2. In any given PCI procedure, the total radiation dose is usually determined by the procedural duration, the duration of fluoroscopy and the number of cine runs taken. Other determinants are dose area product (DAP; the absorbed dose multiplied by the irradiated area) and air kerma (AK; the kinetic energy released per unit mass of air), and complex and longer procedures result in higher radiation exposure for both the primary (PO) and secondary operator (SO)34.
According to the original definition by the International Commission on Radiological Protection, radiation effects were classified into stochastic (random, not dose dependent) and non-stochastic (deterministic, dose dependent). Currently, the classification has been changed to stochastic and tissue reactions, since there is an overlap of common reactions, such as thyroid cancer and cataracts, in both types5. Stochastic injury can result in malignancy, pregnancy complications and inheritable diseases while deterministic injury can cause skin reactions, ocular lens injury and hair loss678. The no-threshold stochastic risk on malignancies implies that there is no such thing as safe radiation exposure, and hence, the use of radiation protection devices deserves sufficient attention.
Radiation exposure in the catheterisation laboratory can be minimised in several ways, including reducing the fluoroscopy and the acquisition times, performing fluoroscopy imaging at the lowest available pulse rate, minimising the number and duration of cine runs, reducing the cine frame rate, amplifying the image size and using collimator beams and filters. The use of radiation shielding equipment like lead caps, a lead apron, gloves, eyewear, a thyroid collar and table lead skirts have also helped to limit the operator-received dose. RADPAD (RADPAD 5100A-O; Worldwide Innovations & Technologies) is a lead-free radiation protection drape containing bismuth and barium as radiation protection materials. When placed appropriately on the patient − between the image intensifier and the operator − it has been shown to reduce the radiation exposure of the PO in routine PCI procedures, transcatheter aortic valve implantation, electrophysiology procedures, and pacemaker and device implantations9101112131415.
Indian data on radiation exposure in the cath lab are limited1617. Almost all previous radiation studies have evaluated the efficacy of RADPAD in reducing radiation exposure to the PO only, and data on its effect on the exposure of the SO during PCI procedures are scarce. Although it is well known that the SO has a lower radiation exposure as compared to the PO due to the SO’s greater distance from the primary beam and the source, the effect of radiation exposure on the SO is also cumulative and hence needs to be assessed.
In this study we aimed to evaluate the efficacy of RADPAD drapes in reducing radiation doses in the cath lab for the primary as well as the secondary operator.
Methods
A total of 160 patients were included in the study (40 with single vessel disease [SVD], 40 with double vessel disease [DVD], 40 with triple vessel disease [TVD], and 40 patients undergoing balloon mitral valvuloplasty [BMV]), randomised in a 1:1 pattern to a procedure with or without the use of RADPAD. The study conformed to institutional ethical guidelines and was conducted between January 2021 and May 2023. Hybrid procedures and procedures requiring a change of operator (during the procedure) were excluded from the study.
The “without RADPAD” group had a “sham” drape in place during their procedures. The sham protective shield and the real protective shield were visually identical, and the primary and secondary operators, patients and cath lab personnel were all blinded to the assigned type of shield.
The disposable protective shield (RADPAD) was positioned on the patient around the sheath insertion point and just caudal to the area covered by the suspended acrylic shield. For all cases involving right radial arterial access, the RADPAD was positioned superior and medial to the sheath insertion point and immediately below the lead shield. For cases involving femoral access, including for BMV, the RADPAD was positioned superior to the sheath insertion point and immediately below the lead shield (Figure 1A). The underlying principle is to place the drape between the primary beam and the PO, ensuring that the drape does not appear in the fluoroscopy image during the procedure.
Standard radiation protection precautions and uniform image acquisition protocols were adopted in all cases. All coronary procedures were done with images acquired at a frame rate of 7.5 frames/s in fluoro mode and 10 frames/s in cine mode. Standard shielding equipment included a lead apron, a thyroid shield and a lead shield suspended from the ceiling between the image intensifier and operator as a part of standard protocol, in both groups. The distance between the image intensifier and the operator varied from 60 cm to 70 cm in posteroanterior (PA) view.
A dosimeter was placed on the upper left side of the chest of the primary and secondary operator in all cases and outside the lead apron (Figure 1B). It was reset to zero at the beginning of each procedure, and the total exposure to the physician was recorded (in mrem) at the end of the procedure. Dosimetry was performed at chest height, outside the lead apron, using a personal dosimeter for the first and second operators (MYDOSE mini PDM-222C-RH and PDM-127B-RH [Hitachi Aloka Medical]). Fluoroscopy times and the total radiation dose as given by the machine (in Gy) were collected for each case. The number of cine runs and the left anterior oblique (LAO)/non-LAO and cranial/caudal angles were also recorded as a part of the secondary analysis.
The operator-received dose (in mrem) was assessed both for the PO and the SO. The primary endpoint was the relative operator exposure, which is the ratio of the operator-received dose (in mrem) to the total radiation (in Gy) recorded at the end of the procedure as given by the machine, with or without RADPAD. The relative operator exposure was compared for all 4 groups with/without RADPAD to assess if RADPAD made a difference in the exposure for simple (SVD) angioplasty versus complex (DVD/TVD, multivessel PCI, bifurcation PCI, left main PCI and chronic total occlusion [CTO] interventions) angioplasty or non-angiographic procedures like BMV.

Figure 1. RADPAD shield position and dosimeter placement. A) The shield is placed on the patient’s arm around the area of sheath insertion and extended medially to the patient’s body. B) The dosimeter is placed on the primary and the secondary operators.
STATISTICAL ANALYSIS
Considering a reduction of 20% in the relative operator exposure as a clinically meaningful difference between procedures with RADPAD and without RADPAD, a sample size of 160 patients was required to obtain a power of 95% chance of detecting significance at the 5% level for a reduction of 20% in the primary outcome measure between the study arms.
The presentation of the categorical variables was provided in the form of number and percentage (%). On the other hand, the quantitative data were presented as the mean±standard deviation (SD) or as the median with 25th and 75th percentiles (interquartile range). Data normality was checked using the Kolmogorov-Smirnov test. For cases in which the data were not normal, we used non-parametric tests. The following statistical tests were applied for the results:
1. The comparison of variables which were quantitative and not normally distributed in nature were analysed using the Mann-Whitney U test (for 2 groups) and the Kruskal-Wallis test (for more than 2 groups).
2. The comparison of variables which were qualitative in nature were analysed using the chi-square test. If any cell had an expected value of less than 5, then Fisher’s exact test was used.
The data were entered into a Microsoft Excel spreadsheet, and the final analysis was carried out using Statistical Package for Social Sciences (SPSS) software, version 25.0 (IBM).
For statistical significance, a p-value of less than 0.05 was considered statistically significant.
Results
The baseline demographic characteristics of the study population, categorised into 4 groups (SVD, DVD, TVD and BMV), are shown in Table 1. Expectedly, the patients in the BMV group were significantly younger (mean age 31.52±11.58 years) as compared to the patients with coronary artery disease (CAD) undergoing PCI (mean age 51.45±15.18 years).
Table 1. Comparison of demographic characteristics between patients with single vessel disease, double vessel disease, triple vessel disease and balloon mitral valvuloplasty.
| Demographic characteristics | Single vessel disease (SVD, n=40) | Double vessel disease (DVD, n=40) | Triple vessel disease (TVD, n=40) | Balloon mitral valvuloplasty (BMV, n=40) | Total (n=160) | p-value |
|---|---|---|---|---|---|---|
| Age, years | 59.02±9.13 | 57.72±10.45 | 57.52±8.26 | 31.52±11.58 | <0.0001* | |
| Male/female | 32/8 | 33/7 | 25/15 | 11/29 | 101/59 | <0.0001† |
| Weight, kg | 65.92±7.09 | 66.20±7.31 | 66.28±8.84 | 53.78±8.90 | <0.0001‡ | |
| BMI, kg/m2 | 23.98±4.91 | 24.21±5.98 | 22.31±6.13 | 19.91±5.12 | ||
| Hypertension | 19 (47.50) | 16 (40.00) | 23 (57.50) | 0 (0) | 58 (36.25) | <0.0001† |
| Diabetes | 24 (60.00) | 24 (60.00) | 26 (65.00) | 0 (0) | 74 (46.25) | <0.0001† |
| Lipids | ||||||
| TC | 170±21.09 | 161±11.55 | 192±21.22 | 110±9.70 | <0.0001† | |
| TG | 156±9.20 | 132±11.30 | 121±12.55 | 76±8.09 | <0.0001† | |
| HDL | 40±5.5 | 32±8.5 | 31±7.5 | 42±9.8 | <0.0001† | |
| LDL | 110±11.56 | 130±12.76 | 111±16.87 | 72±6.56 | <0.0001† | |
| VLDL | 12±5.65 | 11±6.75 | 14±3.77 | 20±6.75 | <0.0001† | |
| Family h/o CAD | 4 (10.00) | 1 (2.50) | 3 (7.50) | 0 (0) | ||
| Current smoking | 11 (27.50) | 12 (30.00) | 7 (17.50) | 0 (0) | 30 (18.75) | <0.0001† |
| Radial approach | 37 (92.50) | 34 (85.00) | 30 (75.00) | 0 (0) | 101 (63.13) | <0.0001† |
| Femoral approach | 3 (7.50) | 6 (15.00) | 10 (25.00) | 40 (100) | 59 (36.88) | <0.0001† |
| H/o ACS | 23 (57.50) | 16 (40.00) | 7 (17.50) | 0 (0) | ||
| CSA | 17 (42.50) | 24 (60.00) | 33 (82.50) | 0 (0) | ||
| Mean fluoroscopy time, min | 15.82±7.28 | 23.95±7.81 | 45.34±10.64 | 26.35±7.98 | 27.86±13.75 | <0.0001§ |
| CTO | 6 (15.00) | 7 (17.50) | 6 (15.00) | 0 (0) | ||
| Bifurcation | 0 (0) | 8 (20.00) | 9 (22.50) | 0 (0) | ||
| Left main | 1 (2.50) | 3 (7.50) | 3 (7.50) | 0 (0) | ||
| Values are expressed as mean±SD, n or n (%). *Fisher’s exact test; †the chi-square test; ‡ANOVA test; §the Kruskal-Wallis test. ACS: acute coronary syndrome; BMI: body mass index; BMV: balloon mitral valvuloplasty; CAD: coronary artery disease; CSA: chronic stable angina; CTO: chronic total occlusion; diff: difference; h/o: history of; HDL: high-density lipoprotein; LDL: low-density lipoprotein; SD: standard deviation; TC: total cholestorol; TG: triglycerides; VLDL: very low-density lipoprotein | ||||||
RADIATION PARAMETERS OF THE FOUR GROUPS OF PATIENTS
The operator-received dose (in mrem) and relative operator exposure for the PO was much higher as compared to the secondary operator, irrespective of RADPAD use, across all 4 groups of patients.
SVDRADPAD versus SVDNoRADPAD
Although the screening times, total radiation dose (Gy) and DAP for SVD patients with RADPAD (SVDRADPAD) versus those without RADPAD (SVDNoRADPAD) was similar, the operator-received dose was significantly higher both for the PO (2.66±1.29 mrem vs 7.92±2.87 mrem; p=0.001) and for the SO (1.08±0.63 mrem vs 5.52±1.47 mrem; p=0.001) when no RADPAD was used (Figure 2, Table 2).
The relative operator exposure both for the PO (1.99±1.70 vs 4.49±2.88; p=0.001) and the SO (0.85±0.72 vs 3.28±2.16; p=0.001) was also significantly higher for those without RADPAD (Figure 3).
The relative operator exposure was also significantly less when the SO used RADPAD versus the PO without RADPAD (0.85±0.72 vs 4.49±2.88; p<0.001)
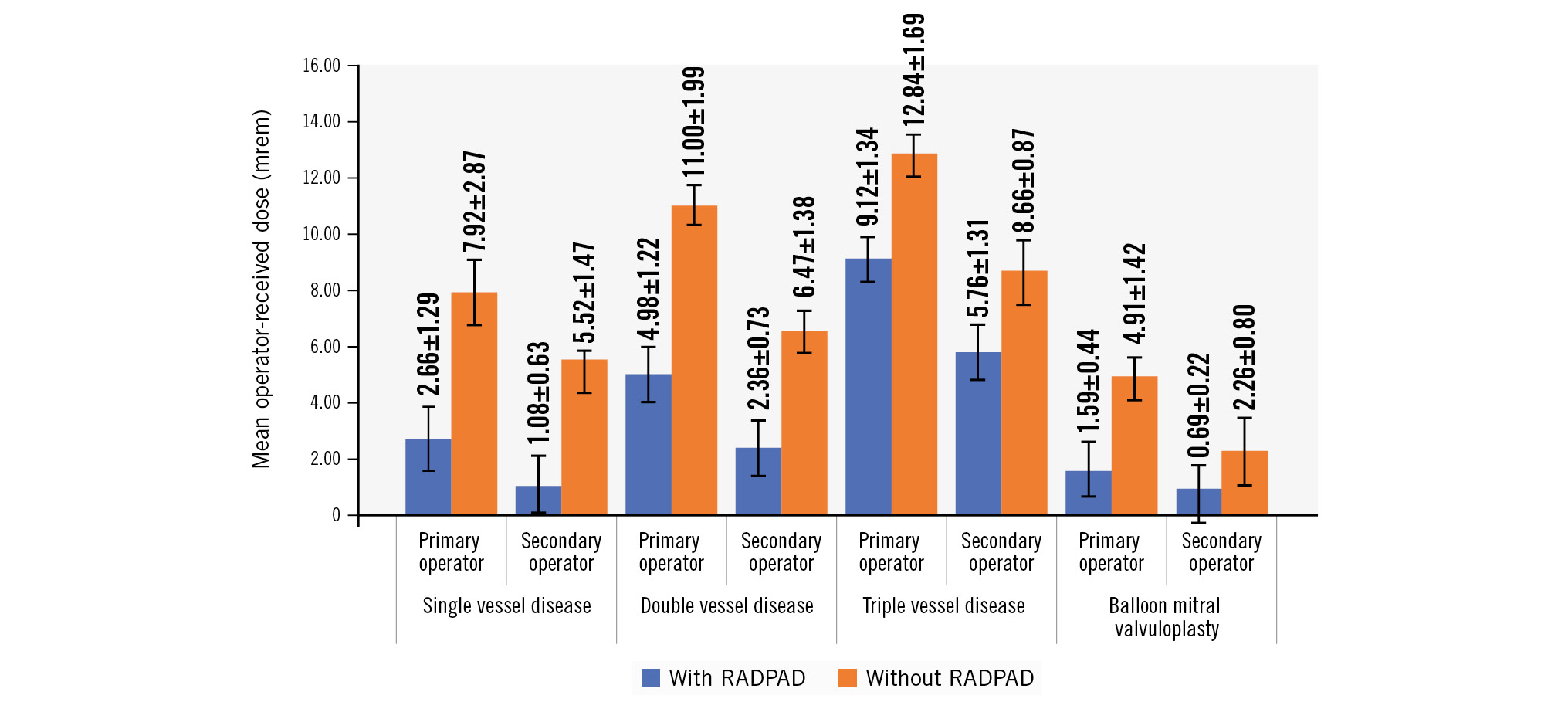
Figure 2. Comparison of operator-received dose (in mrem) for all 4 patient groups, with and without RADPAD.
Table 2. Screening times and radiation exposure parameters for patients with single vessel disease and the primary and secondary operators, with and without RADPAD.
| Parameter | SVDRADPAD | SVDNoRADPAD | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| Screening time, minutes | 13.71±4.42 | 17.93±8.93 | NS¶ | |||||
| Total radiation dose, Gy | 1.91±1.14 | 2.29±1.10 | NS¶ | |||||
| DAP, mGy·cm² | 7,797±5,765 | 6,972±2,813 | NS¶ | |||||
| Parameter | SVDRADPAD | SVDNoRADPAD | p-value | % diff | SVDRADPAD | SVDNoRADPAD | p-value | % diff |
| Primary operator | Secondary operator | |||||||
| Operator-received dose, mrem | 2.66±1.29 | 7.92±2.87 | 0.001¶ | 65% | 1.08±0.63 | 5.52±1.47 | 0.001¶ | 80% |
| Relative operator exposure* | 1.99±1.70 | 4.49±2.88 | 0.001¶ | 55% | 0.85±0.72 | 3.28±2.16 | 0.001¶ | 74% |
| *Relative operator exposure is the ratio of the operator-received dose (mrem) to the total radiation (Gy) recorded at the end of the procedure. ¶The Mann-Whitney U test. Values are expressed as mean±SD unless otherwise stated. DAP: dose area product; diff: difference; NS: non-significant; SD: standard deviation; SVD: single vessel disease; SVDNoRADPAD: SVD patients without RADPAD; SVDRADPAD: SVD patients with RADPAD | ||||||||
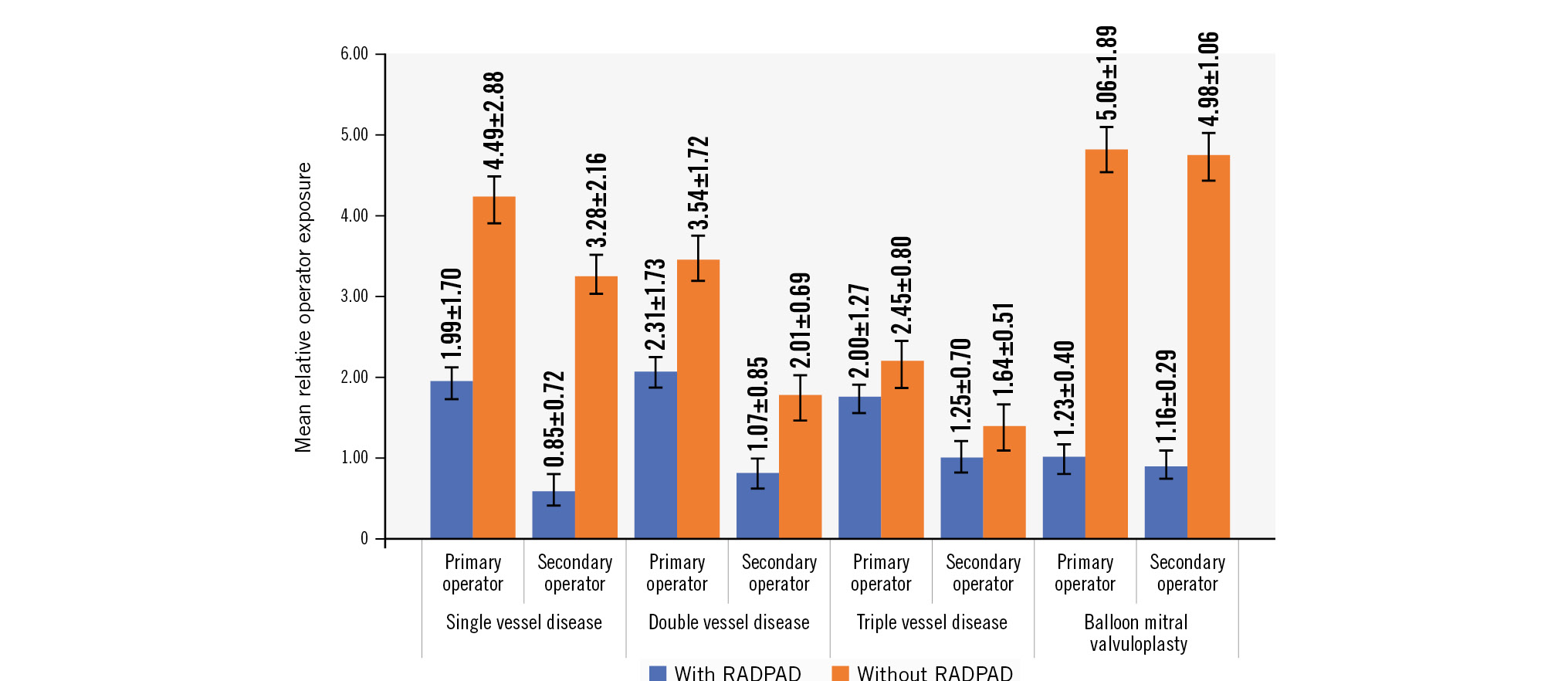
Figure 3. Comparison of relative exposure for all 4 patient groups, with and without RADPAD.
DVDRADPAD VERSUS DVDNORADPAD
Despite similar screening times, total radiation dose (Gy) and DAP for DVD patients using RADPAD (DVDRADPAD) versus DVD patients not using RADPAD (DVDNoRADPAD), the operator-received dose was significantly higher both for the PO (4.98±1.22 mrem vs 11.00±1.99 mrem; p<0.001) and for the SO (2.36±0.73 mrem vs 6.47±1.38 mrem; p<0.001) when no RADPAD was used (Figure 2, Table 3).
The relative operator exposure both for the PO (2.31±1.73 vs 3.54±1.72; p=0.001) and the SO (1.07±0.85 vs 2.01±0.69; p<0.001) was significantly higher for those without RADPAD (Figure 3).
The relative operator exposure of the SO while using RADPAD was significantly lower as compared to the PO without RADPAD (1.07±0.85 vs 3.54±1.72; p<0.001).
Table 3. Screening times and radiation exposure parameters for patients with double vessel disease and the primary and secondary operators, with and without RADPAD.
| Parameter | DVDRADPAD | DVDNoRADPAD | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| Screening time, minutes | 22.66±8.01 | 25.24±7.58 | NS¶ | |||||
| Total radiation dose, Gy | 2.87±1.36 | 3.55±1.18 | NS¶ | |||||
| DAP, mGy·cm2 | 10,356±5,704 | 6,972±3,510 | NS¶ | |||||
| Parameter | DVDRADPAD | DVDNoRADPAD | p-value | % diff | DVDRADPAD | DVDNoRADPAD | p-value | % diff |
| Primary operator | Secondary operator | |||||||
| Operator-received dose, mrem | 4.98±1.22 | 11.00±1.99 | 0.001¶ | 54% | 2.36±0.73 | 6.47±1.38 | 0.001¶ | 63% |
| Relative operator exposure* | 2.31±1.73 | 3.54±1.72 | 0.001¶ | 34% | 1.07±0.85 | 2.01±0.69 | 0.001¶ | 46% |
| *Relative operator exposure is the ratio of the operator-received dose (in mrem) to the total radiation (in Gy) recorded at the end of the procedure. ¶The Mann-Whitney U test. Values are expressed as mean±SD unless otherwise stated. DAP: dose area product; diff: difference; DVD: double vessel disease; DVDNoRADPAD: DVD patients without RADPAD; DVDRADPAD: DVD patients with RADPAD; NS: non-significant; SD: standard deviation | ||||||||
TVDRADPAD VERSUS TVDNORADPAD
The screening times, total radiation dose (Gy) and DAP for TVD patients with RADPAD (TVDRADPAD) versus those without (TVDNoRADPAD) were not significantly different. However, the operator-received dose was significantly higher both for the PO (9.12±1.34 mrem vs 12.84±1.69 mrem; p<0.001) and for the SO (5.76±1.31 mrem vs 8.66±0.87 mrem; p<0.001) when no RADPAD was used (Figure 2, Table 4).
The relative operator exposure both for the PO (2.00±1.27 vs 2.45±0.80; p=0.01) and the SO (1.25±0.74 vs 1.64±0.51; p=0.007) was significantly higher for those without RADPAD (Figure 3).
Similarly, the relative operator exposure of the SO with RADPAD was lower as compared to the PO without RADPAD (1.25±0.74 vs 2.45±0.80; p=0.001).
Table 4. Screening times and radiation exposure parameters for patients with triple vessel disease and the primary and secondary operators, with and without RADPAD.
| Parameter | TVDRADPAD | TVDNoRADPAD | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| Screening time, minutes | 42.91±11.65 | 47.77±9.17 | NS¶ | |||||
| Total radiation dose, Gy | 5.49±1.93 | 5.72±1.76 | NS¶ | |||||
| DAP, mGy·cm2 | 15,894±3,851 | 14,543±4,431 | NS¶ | |||||
| Parameter | TVDRADPAD | TVDNoRADPAD | p-value | % diff | TVDRADPAD | TVDNoRADPAD | p-value | % diff |
| Primary operator | Secondary operator | |||||||
| Operator-received dose, mrem | 9.12±1.34 | 12.84±1.69 | 0.001¶ | 28% | 5.76±1.31 | 8.66±0.87 | 0.001¶ | 33% |
| Relative operator exposure* | 2.00±1.27 | 2.45±0.80 | 0.01¶ | 18% | 1.25±0.74 | 1.64±0.51 | 0.007¶ | 23% |
| *Relative operator exposure is the ratio of the operator-received dose (in mrem) to the total radiation (in Gy) recorded at the end of the procedure. ¶The Mann-Whitney U test. Values are expressed as mean±SD unless otherwise stated. DAP: dose area product; diff: difference; NS: non-significant; SD: standard deviation; TVD: triple vessel disease; TVDNoRADPAD: TVD patients without RADPAD; TVDRADPAD: TVD patients with RADPAD | ||||||||
BMVRADPAD VERSUS BMVNORADPAD
Although BMV does not involve any cineangiography runs (reflecting its much lower total radiation dose [in Gy] as compared to the 3 other groups), the operator-received dose was significantly higher both for the PO (1.59±0.44 mrem vs 4.91±1.42 mrem; p<0.001) and for the secondary operator (0.69±0.22 mrem vs 2.26±0.80 mrem; p<0.001) when no RADPAD was used (Figure 2, Table 5).
The relative operator exposure both for the PO (1.23±0.40 vs 5.06±1.89, p=0.02) and the SO (1.16±0.29 vs 4.98±1.06, p=0.03) was significantly higher for those without RADPAD (Figure 3).
The relative operator exposure of the SO with RADPAD was also lower as compared to the PO when not using RADPAD (1.16±0.29 vs 5.06±1.89; p<0.001).
Figure 4 shows a scatter plot analysis of the total radiation dose (in Gy) to the primary operator-received dose (in mrem) in all 4 groups with or without RADPAD, with a difference between the 2 lines being significant with a p-value of 0.03. Similarly, Figure 5 shows a scatter plot analysis of the total radiation dose to the secondary operator-received dose (in mrem) in all 4 groups with or without RADPAD, with a difference between the two lines being significant with a p-value of 0.001. The findings suggest that RADPAD has a substantial impact on reducing the radiation exposure of both the primary and secondary operator during PCI and BMV procedures.
Table 5. Screening times and radiation exposure parameters for patients undergoing BMV and the primary and secondary operators, with and without RADPAD.
| Parameter | BMVRADPAD | BMVNoRADPAD | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| Screening time, minutes | 24.21±9.7 | 28.49±5.19 | NS¶ | |||||
| Total radiation dose, Gy | 0.56±1.09 | 0.50±0.75 | NS¶ | |||||
| DAP, mGy·cm2 | 4,795±1,596 | 4,967±1,436 | NS¶ | |||||
| Parameter | BMVRADPAD | BMVNoRADPAD | p-value | % diff | BMVRADPAD | BMVNoRADPAD | p-value | % diff |
| Primary operator | Secondary operator | |||||||
| Operator-received dose, mrem | 1.59±0.44 | 4.91±1.42 | 0.001¶ | 67% | 0.69±0.22 | 2.26±0.80 | 0.001¶ | 69% |
| Relative operator exposure* | 1.23±0.40 | 5.06±1.89 | 0.02¶ | 75% | 1.16±0.29 | 4.98±1.06 | 0.03¶ | 76% |
| *Relative operator exposure is the ratio of the operator-received dose (in mrem) to the total radiation (in Gy) recorded at the end of the procedure. ¶The Mann-Whitney U test. Values are expressed as mean±SD unless otherwise stated. BMV: balloon mitral valvuloplasty; BMVNoRADPAD: BMV patients without RADPAD; BMVRADPAD: BMV patients with RADPAD; DAP: dose area product; diff: difference; NS: non-significant; SD: standard deviation | ||||||||
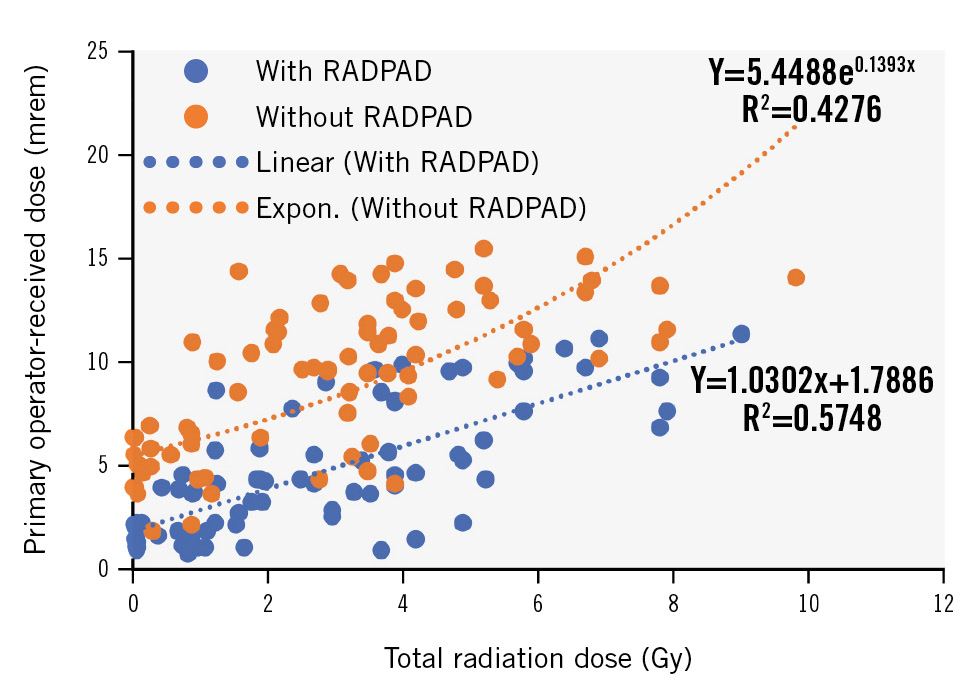
Figure 4. A scatter plot analysis of total radiation dose to primary operator-received dose in each individual case for all 4 patient groups with or without RADPAD. Expon.: exponential
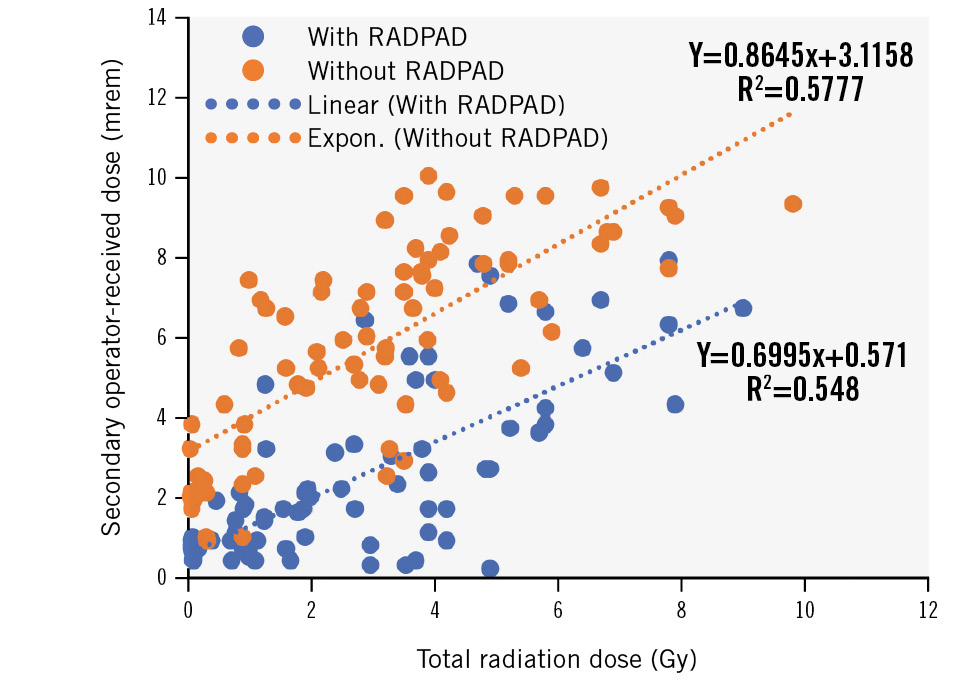
Figure 5. A scatter plot analysis of total radiation dose to secondary operator-received dose in each individual case for all 4 patient groups with or without RADPAD. Expon.: exponential
MEAN RADIATION DOSE PER SHOOT OF RECORDED LAO VERSUS NON-LAO PROJECTIONS
The mean comparison of radiation emitted per second in LAO- versus non-LAO-oriented views revealed significantly higher emitted radiation in LAO caudal-oriented views (7.18±2.48 mGy in cranial view, 11.67±2.68 mGy in caudal view) as compared to non-LAO (4.83±0.87 mGy in cranial view, 4.33±1.12 mGy in caudal-oriented views; p<0.001) (Figure 6).
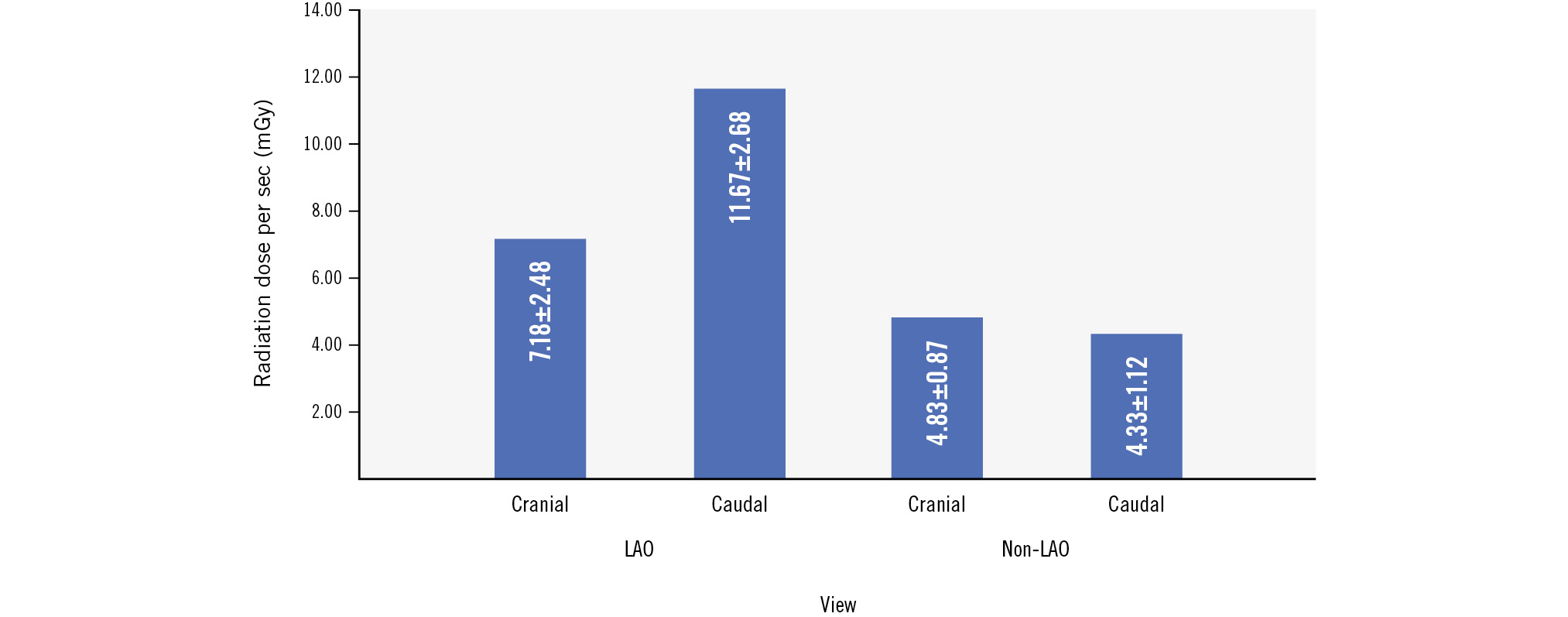
Figure 6. Comparison of radiation dose per second (mGy) in LAO versus non-LAO views. LAO: left anterior oblique
RADIAL VERSUS FEMORAL ROUTE
We noted a higher operator-received dose in radial routes (5.35±2.80 with RADPAD, 10.40±3.04 without RADPAD) as compared to femoral routes (3.30±3.11 with RADPAD, 6.99±3.66 without RADPAD; p=0.04) (Figure 7). Femoral route procedures with RADPAD had a 38% lower operator-received dose compared to the radial cohort.
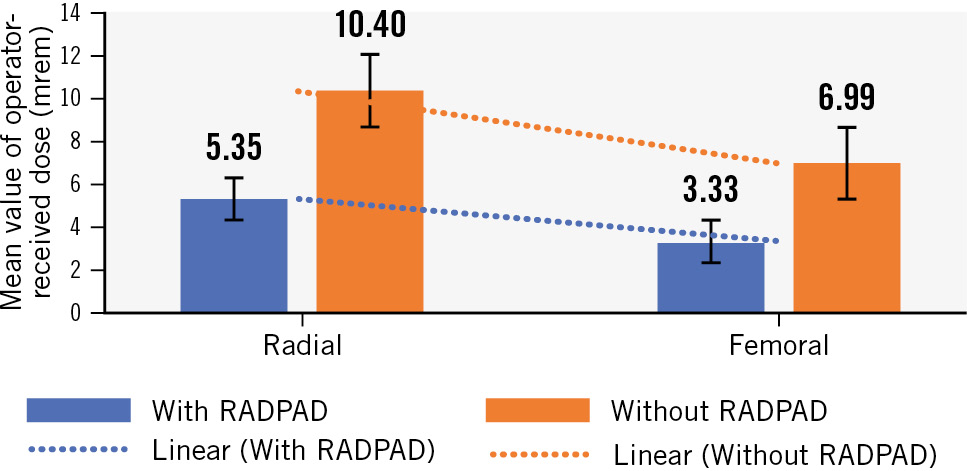
Figure 7. Comparison of operator-received dose in radial versus femoral routes.
Discussion
With the increasing number of cardiac interventional procedures, radiation exposure in the catheterisation lab has become a real concern. Reducing acquisition times, carrying out fluoroscopy imaging at the lowest available pulse rate, using collimation, minimising cine runs, reducing cine frame rates, amplifying image size and using personal protection equipment − like a lead apron, eye goggles, thyroid shield, gloves etc. − help reduce the risk to the operators. RADPAD is a radiation protection drape that has been reported to reduce the amount of radiation absorbed by the PO during various cath lab procedures. Although the exposure reduction of the PO is well described, little data are available regarding its efficacy in reducing radiation exposure to the SO.
In this study of 160 patients, we observed expectedly that with increasing screening times (TVD>DVD>SVD) across the 3 groups of PCI, the operator-received dose (in mrem) and relative operator exposure values increased progressively both for the primary and secondary operators (Figure 2, Figure 3).
EFFECT OF RADPAD USE ON THE RADIATION PARAMETERS OF THE PRIMARY OPERATOR
We observed that the operator-received dose (in mrem) for the PO was significantly less in the RADPAD cohorts across all 4 groups studied (SVD: PO with RADPAD [PORADPAD] vs PO without RADPAD [PONoRADPAD] 2.66±1.29 vs 7.92±2.87; p<0.001; DVD: PORADPAD vs PONoRADPAD 4.98±1.22 vs 11.00±1.99; p<0.001; TVD: PORADPAD vs PONoRADPAD 9.12±1.34 vs 12.84±1.69; p<0.001; and BMV: PORADPAD vs PONoRADPAD 1.59±0.44 vs 4.91±1.42; p<0.001).
For patients with SVD undergoing PCI, use of RADPAD reduced the PO’s received dose (in mrem) by 65% as compared to no use of RADPAD, while the corresponding values for DVD, TVD and BMV were 54%, 28% and 67%, respectively.
The relative operator exposure for the PO (ratio of the operator-received dose to the total radiation [in Gy]) was also significantly less in the RADPAD cohorts across all 4 groups studied (SVD: PO RADPAD vs PONoRADPAD 1.99±1.70 vs 4.49±2.88; p<0.001; DVD: PORADPAD vs PONoRADPAD 2.31±1.73 vs 3.54±1.72; p<0.001; TVD: PORADPAD vs PONoRADPAD 2.00±1.27 vs 2.45±0.80; p=0.01; and BMV: PORADPAD vs PONoRADPAD 1.23±0.40 vs 5.06±1.89; p=0.02).
The overall reduction in relative exposure for the PO was 55%, 34%, 18% and 75%, respectively, for SVD, DVD, TVD and BMV, with the use of RADPAD.
This reduction in radiation exposure for the PO compares well with the previously reported rates of reduction of operator-received scatter radiation in the range of 34-59%910111213141518. The widely variable rates of reduction in these studies are not only related to the diverse patient populations studied (diagnostic angiography as well as various interventional procedures) but also to the site where dosimetry is performed, since the highest attenuation of scatter radiation is obtained at the sites closest to the radiation source, like arms and wrists, compared to dosimetry at chest and eye level111920.
While many of these studies performed dosimetry at the left-arm level, in our study, dosimetry was done at the chest level, as described by Vlastra et al; their study is also the only other study that used a sham-shield arm, as we did in our protocol21. It is important to have a sham-controlled arm in order to actually account for operator radiation behaviour characteristics.
In a previous report by our group, we reported significantly less relative PO exposure with RADPAD (1.39±0.95) versus no RADPAD (2.27±1.40) amounting to a 39% reduction in 65 patients undergoing PCI16. Since there was no sham-controlled arm in that study, in the current study, we not only included a sham arm but also analysed the exposure for both PO and SO.
EXPOSURE FOR THE SECONDARY OPERATOR
Although the SO generally receives 30-50% less exposure to radiation as compared to the PO, it is important to limit the SO’s exposure, since the cumulative effect of radiation exposure can have similar adverse effects as with the PO1422. We observed that the operator-received dose for the SO was much lower as compared to the PO for all 4 groups irrespective of RADPAD use.
A significant reduction in operator-received dose (in mrem) was seen for the SO with RADPAD in all groups of patients (SVD: SO with RADPAD [SORADPAD] vs SO without RADPAD [SONoRADPAD] 1.08±0.63 vs 5.52±1.47; p<0.001; DVD: SORADPAD vs SONoRADPAD 2.36±0.73 vs 6.47±1.38; p<0.001; TVD: SORADPAD vs SONoRADPAD 5.76±1.31 vs 8.66±0.87; p<0.001; and BMV: SORADPAD vs SONoRADPAD 0.69±0.22 vs 2.26±0.80; p<0.001). The % reduction of the SO’s received dose (in mrem) with use of RADPAD was 80%, 63%, 33% and 69%, respectively, for SVD, DVD, TVD and BMV.
The relative operator exposure was also significantly less for the SO as compared to the PO for all 4 groups of patients. A significant reduction in relative operator exposure was seen for the SO with RADPAD in all groups of patients (SVD: SORADPAD vs SONoRADPAD 0.85±0.72 vs 3.28±2.16; p<0.001; DVD: SORADPAD vs SONoRADPAD 1.07±0.85 vs 2.01±0.69; p<0.001; TVD: SORADPAD vs SONoRADPAD 1.25±0.74 vs 1.64±0.51; p=0.07; and BMV: SORADPAD vs SONoRADPAD 1.16±0.29 vs 4.98±1.06; p=0.03). The relative operator exposure of the SO was reduced by 74%, 46%, 23% and 76% in the SVD, DVD, TVD and BMV groups, respectively, with the use of RADPAD.
In the only previous study that assessed exposure to the SO, Bhat et al also reported that RADPAD use significantly reduced the SO’s exposure, and the relative reduction of dose for the SO in the RADPAD cohort was higher as compared to the PO (10-19% higher absolute reduction of radiation to the SO)17. However, unlike our study, the study by Bhat et al had ~40% patients who only underwent coronary angiography, and there was no categorisation of the patient cohort according to the complexity of CAD into SVD, DVD and TVD. We demonstrated that with the increasing complexity of PCI (SVD vs DVD vs TVD) requiring longer screening times, the exposure for both the PO and SO increased, and use of RADPAD provided an incremental benefit.
Limitations
Our study was a single-centre cross-sectional study, and more studies with larger numbers of patients from multiple centres are needed to assess this further. The distance between the operator and the radiation source was not measured during the study and could be a confounder for operator exposure (although it was visually kept constant). The visible presence of the RADPAD could bias the operator and trigger subtle behavioural differences. Moreover, dosimetry at the patient level was also not assessed and could be a focus of interest in future studies.
Conclusions
Our study adds to the scarce Indian data on radiation exposure in the cath lab and shows that the use of RADPAD significantly reduced radiation exposure to both the primary and secondary operator in the range of 39-75%.
It is important for cath lab personnel to always follow the “As Low As Reasonably Achievable” (ALARA) principle to minimise radiation exposure to both patients and themselves. The use of RADPAD, as validated in multiple studies, strongly suggests that it may be incorporated as one of the efficacious best practices in the cath lab along with other techniques to limit radiation exposure.
Impact on daily practice
Our research contributes to the limited body of Indian data concerning radiation exposure in the cath lab. For patients with single, double and triple vessel disease undergoing percutaneous coronary intervention and those undergoing balloon mitral valvuloplasty, the use of RADPAD for the primary operator’s received dose (in mrem) resulted in 65%, 54%, 28% and 67% reductions, respectively, as compared to no use of RADPAD. The % reduction in relative operator exposure for the primary operator for the 4 groups was 55%, 34%, 18% and 75%, respectively, with the use of RADPAD. The corresponding % reductions for the secondary operator’s received dose (in mrem) were 80%, 63%, 33% and 69%, and for relative operator exposure, were 74%, 46%, 23% and 76% in the 4 groups, respectively.
Acknowledgements
We would like to acknowledge and thank all the interventional cardiologists and catheterisation laboratory staff at our institute for contributing to the current trial.
Conflict of interest statement
The authors have no conflicts of interest to declare.

