Severe tortuosity, characterised by one or more bends ≥90°, or three or more bends of 45-90° proximal to the diseased segment in the SYNTAX score calculations, may pose a challenge to wiring and device delivery, thereby increasing the risk of periprocedural complications12. While a steerable microcatheter has been reported as beneficial in the endovascular treatment of cerebral disorders with severe tortuosity3, its application in coronary angioplasty has rarely been reported.
A 69-year-old male with a history of non-ST-elevation myocardial infarction underwent percutaneous coronary intervention (PCI) for a chronic total occlusion (CTO) in the proximal left circumflex (LCx). After a 7 Fr backup-type guiding catheter (Hyperion Super Power Backup [SPB] 3.75 [Asahi Intecc]) and a 5 Fr diagnostic catheter were engaged, bidirectional coronary angiography revealed total occlusion in the proximal LCx with a bifurcation angle >90° from the left main trunk (Figure 1A, Figure 1B). The distal exit of the occlusion was visualised using the Rentrop grade 3 collateral artery from the right coronary artery4.
Attempts to advance the microcatheter (Corsair Pro [Asahi Intecc]) to the LCx was unsuccessful, as it easily prolapsed into the left anterior descending artery (LAD) due to the large bifurcation angle (Figure 1C). We then tried guidewire-crossing using a dual lumen microcatheter (SASUKE [Asahi Intecc]); however, advancing the guidewire to the occlusion was difficult because it similarly prolapsed in the LAD direction when advanced.
To overcome this, we utilised a 2.7 Fr steerable microcatheter (LEONIS Mova [Sumitomo Bakelite]), which allowed the tip to selectively bend towards the LCx (Figure 1D). After carefully deflecting the tip to avoid coronary dissection, the steerable microcatheter was inserted into the LCx and a guidewire (Gaia Next 1 [Asahi Intecc]) was successfully delivered into the total occlusion without prolapse (Figure 1E, Figure 1F). Following successful guidewire crossing (Figure 1G), balloon angioplasty was performed using a 2.5 mm semicompliant balloon. The lesion was then treated with the deployment of a 2.5×18 mm Orsiro stent (Biotronik) (Figure 1H). The total procedural and fluoroscopic times were 150 min and 66.5 min, respectively. The contrast usage during the procedure was 216 ml.
In the clinical setting, guidewire crossing can be particularly challenging in tortuous, severely stenosed, and heavily calcified lesions. To address these challenges, previous studies have recommended using extra backup-type guiding catheters, guidewires with stiffer tips, and extension or dual lumen catheters2. The primary procedural issue in this case was guidewire prolapse due to the large bifurcation angle. Additionally, a strong backup force was required to penetrate the occlusion.
The steerable microcatheter allowed the tip to bend selectively towards the LCx, preventing guidewire prolapse and providing a strong backup force. Similar to our case, previous reports have demonstrated that steerable microcatheters are beneficial in cases involving highly tortuous coronary arteries and enable guidewire navigation to the target lesion without prolapse56. Additionally, they provide a stronger push force due to the reduced reaction force compared to a straight microcatheter. Steerable microcatheters with different variable angles and catheter types (e.g., rapid exchange or over-the-wire) are available6. The LEONIS Mova, used in this case, is an over-the-wire steerable microcatheter that allows up to 180° tip adjustment over 15 mm by using a dial at the proximal end. Although we acknowledge the use of a steerable microcatheter for coronary angioplasty is off label in some countries, our case highlights that it could be a viable option for managing severe tortuosity before reaching the culprit lesion in CTO PCI.
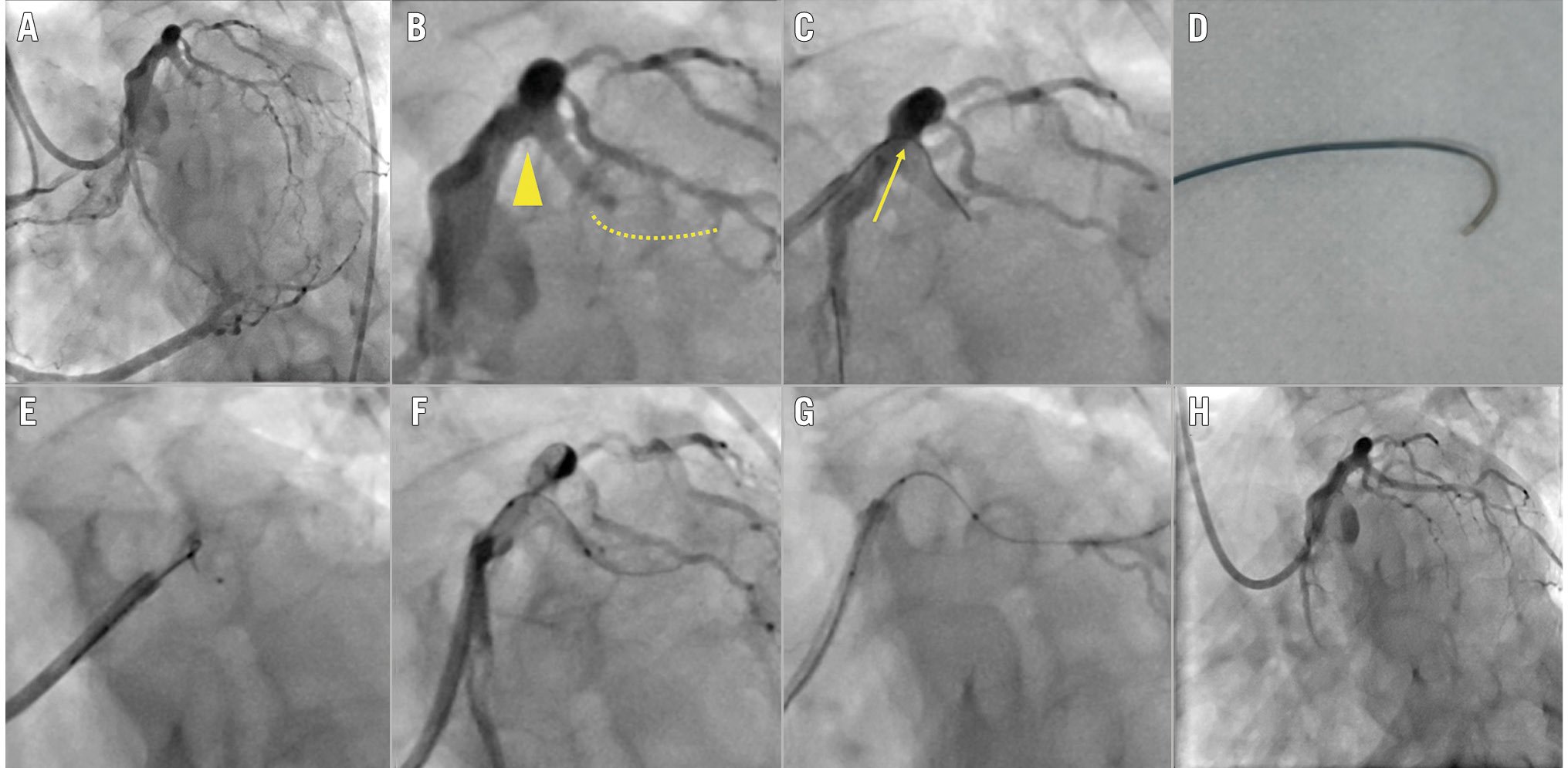
Figure 1. Coronary angiograms during the procedure. A) Bidirectional coronary angiogram showing total occlusion of the proximal left circumflex artery (LCx) with a Rentrop grade 3 collateral artery from the right coronary artery. B) The left main trunk with a bifurcation angle >90° (yellow arrowhead) and total occlusion (yellow dashed line). C) Prolapsed guidewire with a microcatheter in the left anterior descending artery (yellow arrow). D) Steerable microcatheter with a tip bent >90°. E) Steerable microcatheter advanced to the proximal LCx. F) Guidewire penetrating the occlusion through the steerable microcatheter. G) Successful guidewire crossing through the occlusion. H) Final angiogram after stent deployment.
Conflict of interest statement
The authors have no conflicts of interest to declare.

