Introduction
The rapid increase in cardiovascular disease is well documented, with an estimated 64 million new patients since the year 20151. Though there are no accurate estimates of ST-elevation myocardial infarction (STEMI) cases in India, experts put a figure upwards of 3 million a year. Over the last few decades, significant advances in the treatment of STEMI have been made, resulting in a considerable decrease in overall mortality and morbidity. However, this progress is not uniform due to vast racial, ethnic, economic and gender related disparities in resource utilisation, and the availability of prompt revascularisation2. Irregularities in access to health care and timely treatment are mostly due to a complex interplay of personal, socioeconomic, environmental and lifestyle choices, along with contemporary organisational gaps. Addressing these disparities in STEMI health care is important, not only from the perspective of social uniformity, but also for improving the nation’s overall health and productivity. The successful use of systems and treatment protocols hold the potential to standardise health care for all. Developing systems of STEMI care in India is a challenge because of the complexities involved in allocating scarce health care resources, which should be effective and equitable, along with the lack of adequate infrastructure and trained workforce. Finally, the disproportionately high prevalence of acute coronary syndromes (ACS) in the lower socioeconomic classes and the consequent higher mortality due to poor access to quality health care, makes it imperative that any system devised should ensure equity, so that no patient falls through the system due to high costs.
Guidelines from most of the reputed societies emphasise the dominant role of primary percutaneous coronary intervention (PCI) as the reperfusion strategy to be followed in STEMI patients. However, inaccessibility to cardiac catheterisation laboratories (cath labs) and transport delays have restricted primary PCI to only a small proportion of eligible patients. Data from the ACCESS registry from Africa, Latin America and the Middle East3 and the CREATE registry data from India4 show that a substantial proportion of patients do not receive any form of reperfusion. Furthermore, primary PCI is seldom used as the means for reperfusion in most low- and middle-income countries (LMIC). Thrombolysis is the main mode of reperfusion and is almost always used as a stand-alone treatment. The recent data supporting the use of the pharmacoinvasive (PI) strategy as a reasonable option for treating STEMI patients has opened a window of opportunity in delivering a more practical and effective reperfusion treatment for the majority of patients from LMICs56.
STEMI India
Origins and rationale for an organisation focused on STEMI management
Although STEMI meetings have been held in India in the past, they have been sporadic and mainly target cardiologists. The first concrete attempt to run a STEMI meeting and train all medical personnel, including physicians and general practitioners involved in thrombolysis, as well as cardiologists involved in primary PCI, was made when the first Kovai Lumen meeting was organised at Coimbatore, Tamil Nadu in 2010. It was modelled after the “Lumen” conference, conducted in Miami, and separate workshops were run in parallel to train paramedics, nurses, emergency room physicians and cardiologists. While this meeting served the purpose of educating medical teams in hospitals, it was felt that in order to have an impact on the management of STEMI across the country, a national organisation dedicated to all aspects of STEMI management was needed. At the 2010 annual meeting for cardiologists held in Calcutta, the decision was made to set up STEMI India, a not-for-profit organisation. The organisation was registered in February 2011.
Goals of STEMI India
STEMI India aims to advance the field of STEMI management by imparting and disseminating the latest international information on STEMI management to all those involved in STEMI care. The annual STEMI India meeting brings together experts in the field from around the world. The unique aspect of the meeting is that it lays equal emphasis on thrombolysis, PI strategy and primary PCI, since all three modalities of reperfusion have a role in India and other LMIC.
The need to develop STEMI systems of care relevant to India, and to work towards a national STEMI program, was another very important goal. The recent white paper on resource- and infrastructure-appropriate management of STEMI in LMIC7 is a landmark paper that can guide countries with resource constraints on how to manage STEMI. The lack of adequate research data on STEMI from LMIC is a major constraint in planning appropriate programs. STEMI India aims to help organisations and individuals in research projects by sharing expertise. To date, the organisation has published over 15 papers in leading journals from across the world, significantly contributing to advancements in the field.
Developing a system of care for STEMI
Data from the National Interventional Council show that there is a trend towards increasing primary PCI in India in recent years for the treatment of STEMI. The overall percentage of primary PCI remains insignificant, however, when the total STEMI burden of the country is considered8. The recent STREAM (STrategic Reperfusion Early After Myocardial infarction) data6 and the Indian data from the STEP-PAMI study5 showed that the PI strategy compared well with primary PCI in overall morbidity and mortality. Based on this evidence and the success of the Pilot STEMI-Kovai Erode study9, STEMI India proposed that STEMI management in India adopts the dual strategy of combining primary PCI with PI reperfusion to develop a coherent framework for developing a system of care, referred to as the STEMI India Model:
- Primary PCI for patients located close to cardiac cath labs. Such an option would be available mostly for patients in urban areas with a presumably short transportation time to hospitals equipped with 24/7 primary PCI capabilities.
- Patients in rural areas, with suspected long transportation times to PCI-capable hospitals, would utilise the PI strategy with thrombolysis therapy, followed by catheterisation and PCI, if indicated, within 3-24 hours of thrombolysis.
The architecture of this system is based on a hub-and-spoke model, with each set of networked hospitals dubbed a “STEMI cluster”.
The Tamil Nadu STEMI project – the validation study
The Tamil Nadu STEMI project was rolled out to assess the feasibility of developing a system of care for STEMI in 4 clusters across the southern Indian state of Tamil Nadu using the model developed by STEMI India10.
Hub-and-spoke hospitals from different areas (metropolitan, urban and rural) and different systems (public, corporate and charitable hospitals) were included. All hospitals were accredited by the state health insurance program to eliminate out-of-pocket payments, ensuring that virtually no patient in the system would be denied treatment due to lack of finances. The Emergency Medical Research Institute (EMRI) ambulance system, an essential partner in the project, had a clear mandate to move a STEMI patient picked up in the region to the closest STEMI hospital in the cluster.
The results of this study demonstrated the feasibility of developing a successful system of care to manage patients with STEMI11. Incorporating state-of-the-art technology and standardised protocols into systems of care helped in providing reperfusion. Access to the PI strategy increased from 3% to 30%, especially for patients from rural areas who traditionally received stand-alone thrombolysis as the only treatment for STEMI11. One-year mortality dropped by 19% relative to the pre-implementation cohort, reinforcing the fact that the pharmacoinvasive method is a superior treatment strategy. The STEMI India Model was also proven to be cost effective with a cost-benefit ratio of 3.9812.
STEMI India Model – variants tailored ACCORDING TO infrastructure and workforce availability
Considering the diverse needs of different LMIC, STEMI India has migrated to a 3-model framework for implementation. These 3 models are based on the infrastructure and workforce availability. Upon completion of the geographic and cluster mapping, and depending on the unique characteristics of the region, the appropriate STEMI Model is chosen.
Model 1
The thrombolysis-only model
When a region has no tertiary care centres with a cath lab within 2 hours driving distance of the hospitals, the thrombolysis-only model is chosen (Figure 1).
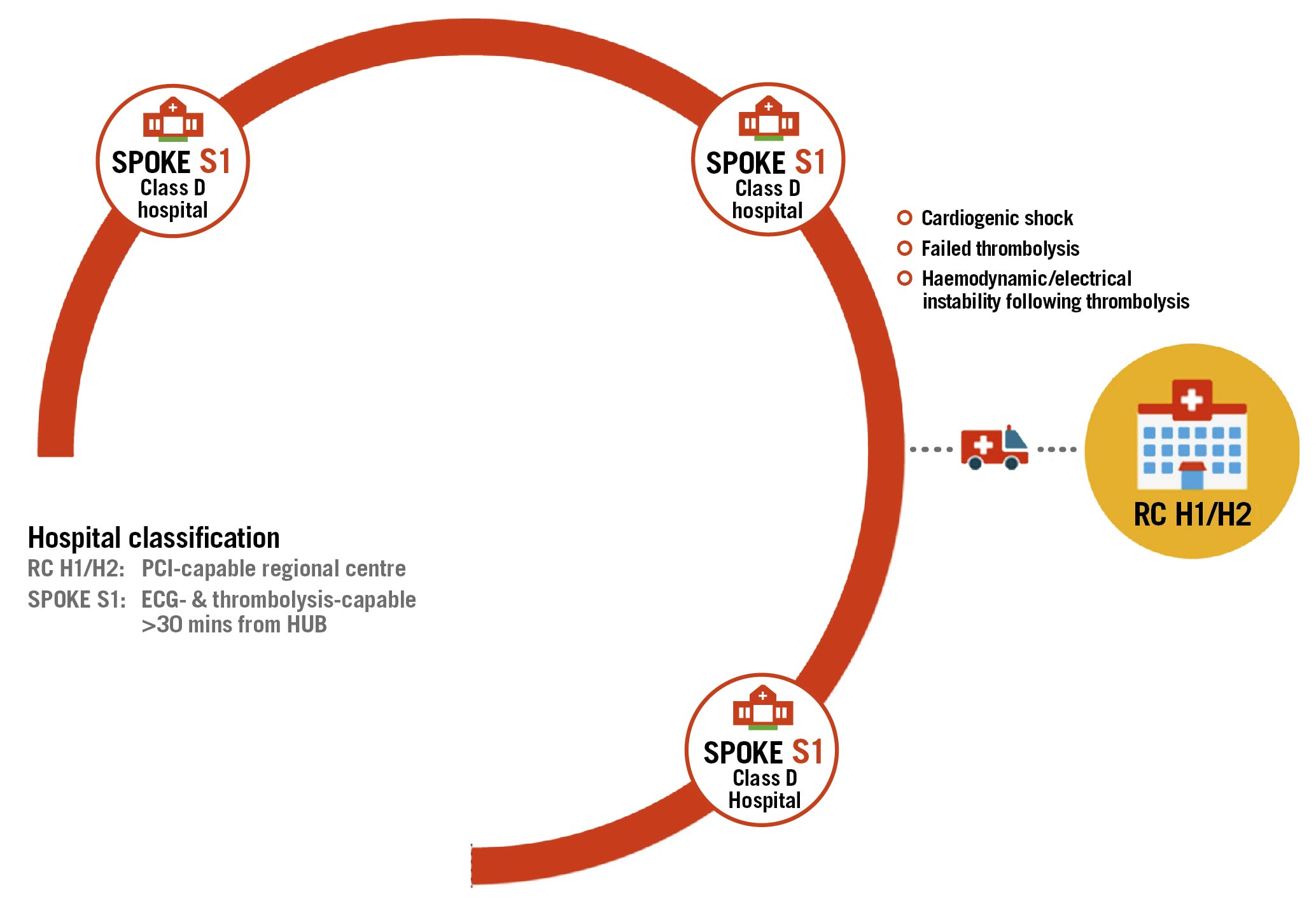
Figure 1. The thrombolysis-only model.
- Up to 15 thrombolysis capable (S1) hospitals form a cluster
- Electrocardiogram (ECG) machines and the necessary equipment and software for monitoring and connectivity are installed in hospitals and ambulances
- Periodic and continuous training is provided on protocols and the use of devices, diagnosis and management of STEMI
- The nearest hospital with a cath lab is allocated as a regional centre where the patient can be transferred via the emergency services ambulance for conditions such as:
- cardiogenic shock
- failed thrombolysis
- haemodynamic/electrical instability following thrombolysis
One variant of Model 1 is a tele-ECG model, Model 1a, for clusters where remote diagnosis of ECGs is required. The ECG machines in these spokes are capable of transmitting ECGs via secure servers for telediagnosis. A second variant is Model 1b, a tele-CCU model, where complete handholding of patient management is provided through the necessary audio-visual and monitoring equipment.
Model 2
The pharmacoinvasive STEMI India model
This is the classic STEMI India model that was validated in the Tamil Nadu STEMI project. It is implemented in regions where a tertiary care centre with a cath lab is located within 2 hours driving distance of the spoke hospitals (Figure 2).
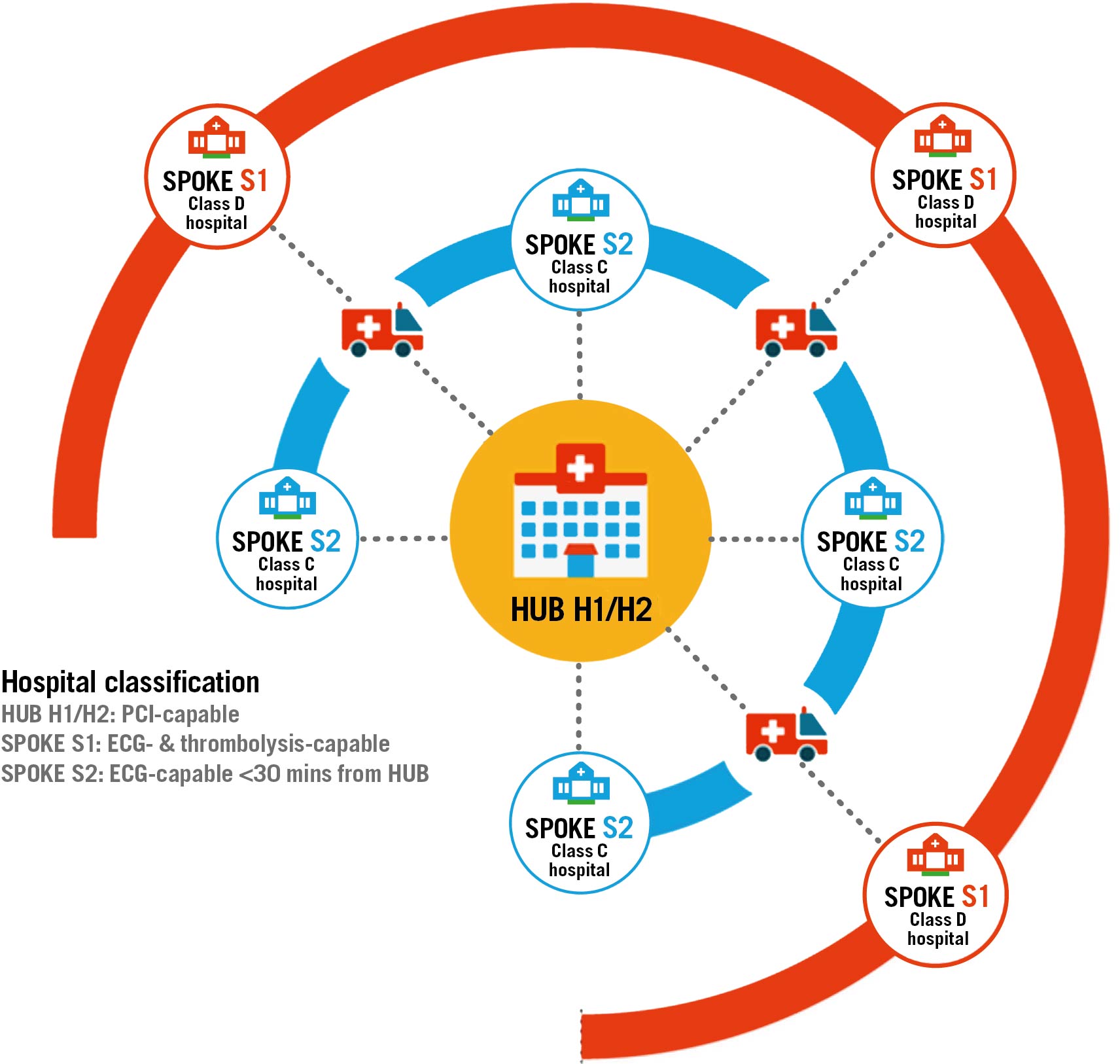
Figure 2. The pharmacoinvasive STEMI India model.
- Up to 15 thrombolysis-capable (S1)/ECG-capable (S2) hospitals linked to a tertiary care centre with a cath lab (H1/H2) form a STEMI cluster
- ECG machines and the necessary equipment and software for monitoring and connectivity are installed in hospitals and ambulances
- Periodic and continuous training is provided on protocols and the use of devices, diagnosis and management of STEMI
- Tele-ECG support is provided in case of a delayed response from the on-call cardiologist at the hub hospital
- All patients are treated with the superior strategies of primary PCI or the PI approach.
A variant of this model, Model 2a, is available for regions with 2 tertiary care centres, with cath labs close to each other and located within 2 hours driving distance of the spoke hospitals, with both included in the same cluster (a “dual-hub” cluster).
Model 3
The primary PCI STEMI India model
Model 3 is implemented when a region has a tertiary care centre with a cath lab within 30 minutes driving distance of ECG-capable hospitals and there are no thrombolysis-capable hospitals in the area participating in the cluster. These clusters will be located primarily in large metropolitan areas with multiple PCI-capable hospitals (Figure 3).
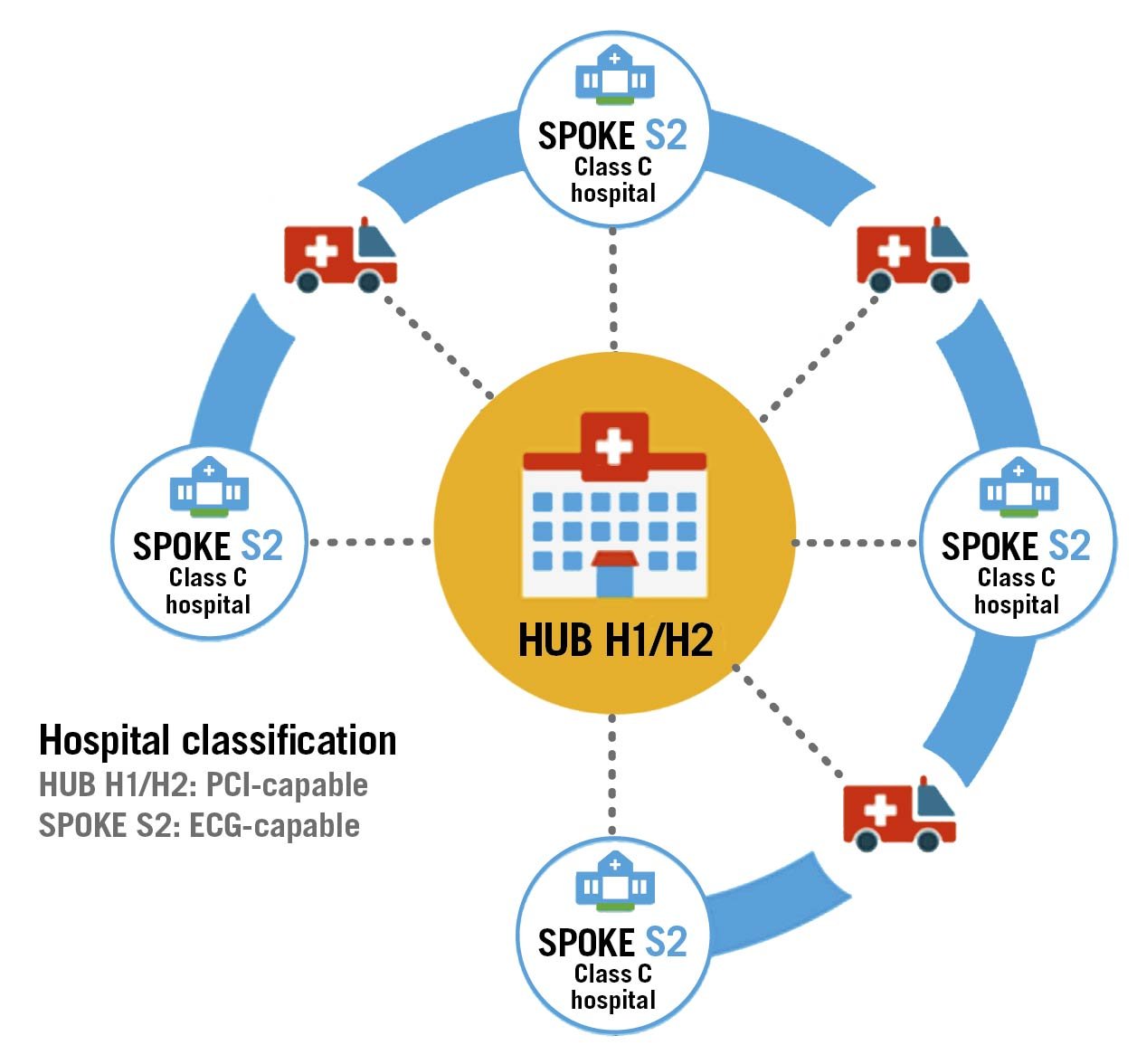
Figure 3. The primary PCI STEMI India model.
- Up to 15 ECG-capable (S2) hospitals linked to a tertiary care centre with a cath lab (H1/H2) form a STEMI cluster
- ECG machines and the necessary equipment and software for monitoring and connectivity are installed in hospitals and ambulances
- Periodic and continuous training is provided on protocols and the use of devices, diagnosis and management of STEMI
- Tele-ECG support can be provided in case of a delayed response from the on-call cardiologist at the hub hospital
All patients diagnosed with STEMI at the spokes (S2) are immediately transferred in appropriately equipped ambulances.
Developing a consensus on the framework for an appropriate STEMI program in India
Based on the success of the Tamil Nadu STEMI project, STEMI India developed a framework for establishing a nationwide system of care for STEMI, which has been endorsed by the Cardiological Society of India (CSI) and the Association of Physicians of India (API)13. Effective infrastructure and a clear partnership among key stakeholders are essential for a successful STEMI program, along with the full support and involvement of the State Government. Social insurance to cover the population below the poverty line, ambulance services that ensure safe transportation across the network, and participation of public hospitals in a STEMI program are crucial to its success in bringing about equitable access to care.
The other important areas are:
- Legislation to accredit STEMI hospitals and prescribe minimum training requirements, infrastructure requirements and workforce requirements to handle STEMI patients
- Legislation for emergency medical services (EMS) to bypass non-STEMI hospitals and transport patients to STEMI-accredited hospitals for management
- Regulation of new STEMI hospitals within systems of care, so that there is an even distribution of STEMI hospitals.
The participation of cardiologists at the hub hospitals as well as that of the physicians at the spoke hospitals in the training of STEMI protocols is essential. Public engagement to educate patients about symptoms of concern and the availability of STEMI services will also ensure that patients access the right point-of-care soon after symptom onset.
The digital tools, protocols and manuals used during the Tamil Nadu STEMI project have already been developed and tested. Technical know-how and training programs are also available for use. These may be modified as required, based on local needs, and in consultation with the local state partners. STEMI India also has the capability to map, develop and run the STEMI program in any state, in collaboration with local partners. In addition, technology and telecommunication networks can provide crucial input that will help overcome many of the infrastructure and workforce deficiencies that exist in LMIC.
Expanding the reach of the program
Other states in India
The National Health Mission, Gujarat has commissioned STEMI India to implement the STEMI India Protocol in U. N. Mehta Institute of Cardiology & Research Centre and in 6 spoke hospitals in and around Ahmedabad from 2019 onwards. The classic hub-and-spoke model, Model 2, was implemented. A total of 2,604 patients were registered up to March 2021, 1,511 of whom made first medical contact with one of the spokes. Patient transfers to the hub increased from about 20% of all spoke patients prior to implementation, to 88% by February 2021 (yet to be published data).
In the northwestern state of Punjab, STEMI India implemented the STEMI India Protocol – model 2 in the region surrounding the Hero DMC Heart Institute, Ludhiana, between 2018 and 2020. Fifteen spoke hospitals participated and 1,712 STEMI patients were registered, 773 of whom made first medical contact at one of the spokes or an external hospital. Treatment strategies improved, with the “no treatment” subset decreasing, and primary PCI as well as the PI strategy showing a remarkable increase (23% to 40% pre- versus post-implementation). Preliminary analysis of the 1-year outcomes shows a significant reduction in mortality (yet to be published data).
In Jharkhand, the National Health Mission has instituted 10 spokes with no facility for thrombolysis as part of the cluster. STEMI India is working with the Government to upgrade them into thrombolysis-capable centres with Model 1a, remote diagnosis of ECGs, being adopted here.
Many other states are in the process of starting similar programs, with a slight delay in implementation due to the onset of the COVID-19 pandemic. Discussions are taking place in Andhra Pradesh, Karnataka, Chhattisgarh and Tripura to roll out STEMI programs customised to the unique requirements of each state.
International collaboration and projects in other LMIC
The STEMI India program has garnered great interest in countries across the world. Presentations at major meetings around the world have helped to showcase the model and the feasibility of running similar programs in LMIC.
A white paper on developing STEMI networks in LMIC, authored by leading cardiologists with an interest in STEMI management around the world was published in Circulation11, and has been endorsed by many leading medical organisations. This paper highlighted a way for these countries to develop infrastructure- and workforce-appropriate models which could be seamlessly upgraded with improvements in facilities and the workforce. The STEMI India Model and its variants, modified to suit individual country requirements, was highlighted as the ideal system of care for these countries. A similar paper in EuroIntervention14, authored by members of the Stent – Save a Life (SSL) organisation, also highlighted this model.
It is clear that the digital tools and training modules developed by STEMI India, as well as the protocols and treatment pathways for different levels, could be used to run this program in different resource-challenged regions.
The STEMI India software is currently being used in South Africa as a registry, initially for data collection, and subsequently to enable the roll-out of a system of care.
SSL is a Paris-based global organisation that is affiliated with EuroPCR, with 31 member countries. The current focus of the organisation is to help LMIC improve STEMI management and help them develop STEMI networks. SSL has now signed a memorandum of understanding with STEMI India to utilise their expertise and digital tools to help run these programs in different countries. As an initial proposal, 3 countries in Africa have been chosen and STEMI India will implement the STEMI India Model in these countries.
The way forward
India has almost twice as many private hospitals than public hospitals, and the private hospitals have 50% more ICU beds than are available in the public sector15. Total private infrastructure accounts for 60-70% of the total health infrastructure in the country15. Unfortunately, there is a glaring lack of participation by private hospitals in any organised STEMI network. The impetus for this could come from government regulations or insurance companies. Legislation, similar to that for road traffic accidents, which mandates immediate treatment in private hospitals with payment for those below poverty level from the Government health insurance program, could be a solution. The situation is similar in other LMIC.
The collaboration of STEMI India and SSL opens the door to globalise this model in LMIC. The first steps to implement similar programs in Africa have started, and with the global reach of SSL and EuroPCR, this could be a critical step to help countries to develop a much-needed STEMI network.
The COVID-19 pandemic has slowed down or even stopped implementation of these programs in many states. This has primarily been due to diversion of manpower and resources away from non-communicable disease (NCD) programs such as STEMI and moved to managing the pandemic. This has also been the situation in many other countries in Asia and Africa who were ready to start similar programs. It is hoped that once the pandemic subsides, there will be a restoration of funding and prioritisation of NCD in government programs.
Though these programs have been conducted in different states and countries by STEMI India, it is hoped that eventually these programs will be taken over and run by the local governments. STEMI India can and will continue to support these programs by offering the use of its digital tools, protocols and training programs, but for the long-term sustainability of such programs, there has to be ownership by the local stakeholders and close cooperation of the public and private healthcare sectors.
Conflict of interest statement
The authors have no conflicts of interest to declare.
