A 72-year-old male with a history of hypertension and dyslipidaemia presented to our hospital with acute chest pain. He had begun to feel the pain while climbing stairs and called an ambulance when it was not relieved by rest. He was transported to our hospital and examined in the emergency room. He was haemodynamically stable without any particular signs on the physical exam. ST-elevation was seen in V1-3 on electrocardiogram, and, therefore, with the acute chest pain, ST-segment elevation myocardial infarction was suspected. He was immediately transferred to the catheterisation laboratory for emergency coronary angiography (CAG).
CAG showed 99% stenosis in the proximal segment of the left anterior descending artery. We considered it to be the culprit lesion and subsequently performed an angioplasty.
Since it was a bifurcation lesion, we deployed the jailed balloon technique to avoid the risk of acute side branch occlusion (Figure 1A). After we implanted the stent, we assessed the lesion with intravascular ultrasound (IVUS) and found that the stent was partially underexpanded near the proximal edge. Thus, post-dilatation of the stent was performed with a non-compliant balloon (Figure 1B). After the post-dilatation, angiographic coronary flow was successfully restored (Thrombolysis in Myocardial Infarction [TIMI] grade 3) (Figure 1C) and we removed the guidewire from the side branch. We reassessed the target lesion with IVUS, but it was difficult to evaluate the stent apposition (Figure 1D) and, therefore, we decided to use optical coherence tomography (OCT). With the high-resolution image provided by OCT, we unexpectedly came across a foreign body while crossing the target lesion (Figure 1E, Moving image 1). We considered the possibility of this being a thrombus and decided to apply angioscopy to eliminate the risk of acute stent thrombosis. Under angioscopy we observed a greenish-yellow structure looped around or through the stent, conceivably the coating of a protection guidewire, which may have been rubbed off due to friction between the newly placed stent and the arterial wall as it was pulled out (Figure 1F, Moving image 2). We decided it was not clinically significant and concluded the procedure.
In the case of a bifurcation lesion, side branch protection is considerably important, as acute side branch occlusion increases the rate of major adverse cardiovascular events1. There are several techniques proposed to protect the side branch, such as the jailed wire technique, jailed balloon technique, and jailed corsair technique. The jailed balloon technique might be better than the jailed wire technique in avoiding the acute side branch occlusion2. In this patient we deployed the jailed balloon technique, and percutaneous coronary intervention was successful.
We could not visualise the foreign body with IVUS, but it was easily detectable with OCT and relatively well visualised with angioscopy.
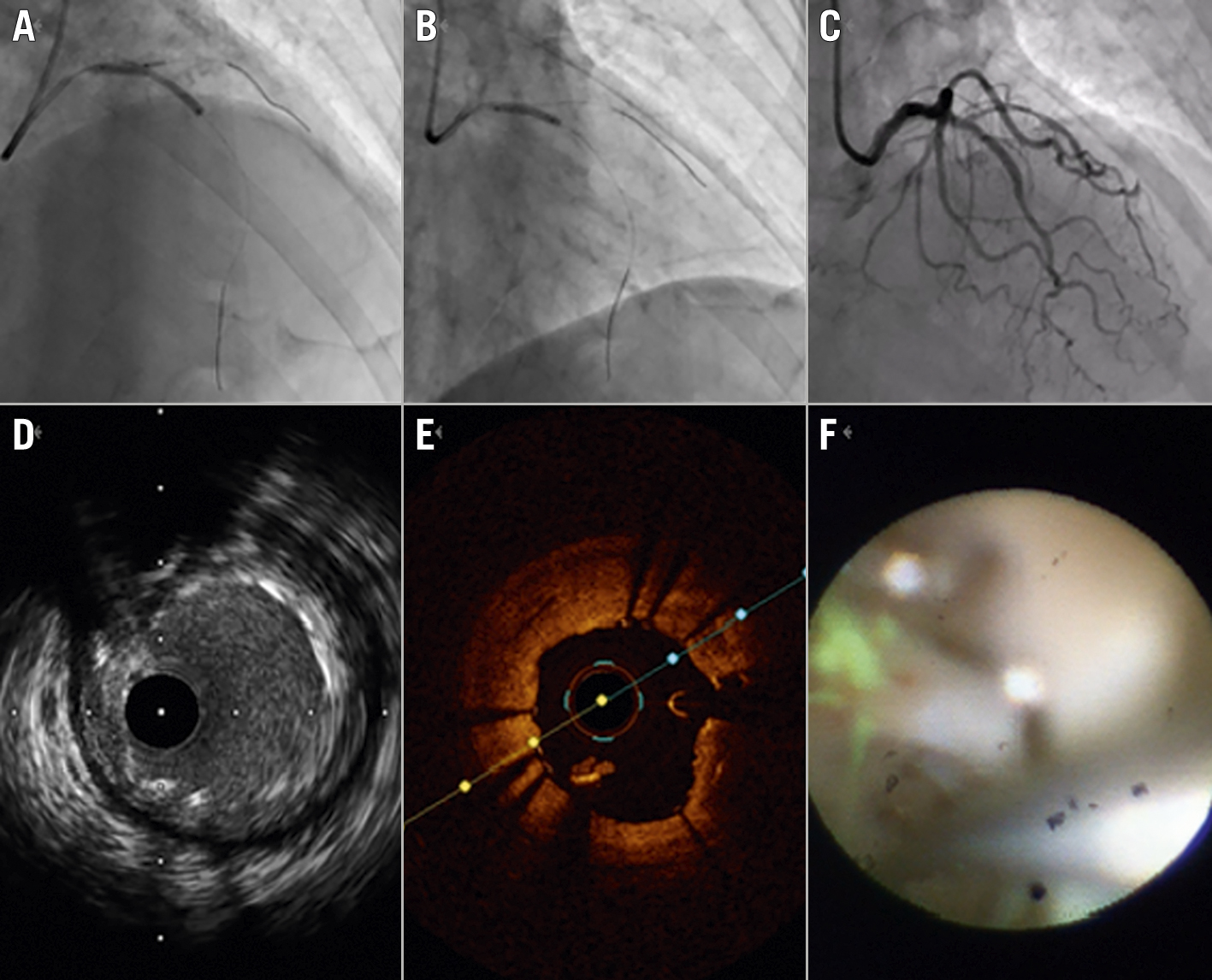
Figure 1. Percutaneous coronary intervention. A) Jailed balloon technique. B) Post-dilation. C) Final angiogram. D) IVUS image. E) OCT image of the same site. F) Angioscopy showing a greenish-yellow structure looped around or through the stent. IVUS: intravascular ultrasound; OCT: optical coherence tomography
Conflict of interest statement
The authors have no conflicts of interest to declare.

